Cystectomy
Pre/Post-Op Cystectomy Management
ERAS Preop
- Provide resources to understand disease and connect with others (BCAN)
- Correct anemia, nutritional deficiencies
- Encourage smoking cessation and alcohol reduction 4 weeks before surgery
- No need for mechanical bowel preparation
- Encourage preoperative carbohydrate loading
- Ingest solids up to 6 hours before surgery, clear liquids up to 2 hours before surgery
- Give preoperative lovenox, use SCDs
- Avoid intraoperative hypothermia
- Perform pre-op stoma marking
Surgical Risks/Expectations
- Pain
- Bleeding
- Infection (5-39%)
- Injury to organs
- Ileus (2-32%)
- Issues w/ diversion (up to 33%)
- Impotence (40%)
- Recurrence (see below)
- Readmission (10-30%)
- Mortality (3% - 4-6% if > 75yo)
Ileal conduit complications
- Urine leak: 2%
- Infection: wound infection (2-7%), abscess (2%), sepsis (3%), pyelonephritis (3-18%)
- Wound dehiscence: 3%
- Obstruction: ileus (6%), intestinal obstruction (3-5%), ureteral obstruction (2-6%)
- Stoma: hernia (2%), stenosis (3%)
- Metabolic: acidosis (13%), stones (7%), renal failure (7%)
- Conduit bleeding (4-10%)
Robotic Cystectomy
Prepping
- General anesthesia, a-line, ceftriaxone
- Postioning: either split leg or supine (depends on robot)
- Tuck arms at sides
- Prep from xiphoid to genitals
- Trendeleberg 23deg, do not flex/rotate bed
Access
- Place veress at umbilicus, insufflate
- Ports: 8mm superior to umbilicus at midline (midline incision), 8mm robot ports x2 on patient's R side, 8mm robot port x1 on patient's L side, 12mm assist on lateral L side, 12mm assist superior and triangulated with midline and L robot ports
- Robot instruments: bipolar forceps in Arm #1, camera in Arm #2, monopolar scissors in Arm #3, forceps in Arm #4
Visibility and posterior access
- Identify and take down any physiologic adhesions holding bowel in the pelvis
- Widely incise peritoneum posterior to bladder (1 instrument-length above rectum), open upwards as smiley-face
- Identify and retract seminal vesicles anteriorly, develop space posterior to prostate up to the apex
Lateral dissections
- Identify ureter at bifurcation of iliac vessels, open peritoneum overlying ureters
- Isolate ureter (keep periureteral fascia intact), trace towards bladder, cut attachments at leading edge
- Once ureter traced down to bladder, place clips x2 (proximal clip tagged), then divide between with cautery
- Divide peritoneum lateral to the medial umbilical ligament (obliterated umbilical artery)
- Enlarge the space, define the plane between perivesical fat and preperitoneal fat
- Should not be able to identify bladder, iliac vessels, or obturator nerve if in correct planes
- Connect peritoneal incisions together, divide vas with cautery once identified
- Superior plane/dissection is completed when endopelvic fascia identified
- For bladder/prostate pedicle, clip the medial umbilical ligament and other larger vessels prior to dividing, otherwise divide with bipolar and cautery, trace along prostate (do not dive into rectum)
Anterior dissection
- Divide medial umbilical ligaments close to abdominal wall to drop bladder completely
- Divide anterior prostatic attachments, then place DVC stitch transversely x2-3, use perineal pressure if needed
- Place clip on urethra, divide distal to clip to completely separate specimen and prevent tumor spillage
Pelvic LND
- Identify external iliac artery, split tissue over the artery and begin to peel medially
- Continue peeling medially, peel off the internal iliac vein
- Continue dissecting out of the obturator fossa, bipolar perforating vessels
- Identify obturator nerve and separate from the tissue
- Divide tissue from distal attachments and proximally near bifurcation
- Remove lateral tissue off iliac artery and from overlying the psoas muscle up to genitofemoral nerve
Finish robotic portion
- Apply hemostatic agents
- Place specimens in a bag
- Create window below sigmoid mesentery without getting into presacral space (stay on top of iliac bifurcation)
- Bring left ureter through window to R side
- Place drain through L side assist port
- Undock robot, remove ports
Create the conduit
- enlarge midline port, travelling to L side of umbilicus (away from stoma)
- Remove specimens and place hemostats on ureters
- Identify 20cm terminal ileum, at least 10-20cm proximal to ileocecal valve, mark ends with silk suture
- Shine light through mesentery, create window with bovie, then enlarge with ligasure
- Staple to divide proximal and distal ends
- Cut off antimesenteric corner of bowel ends, staple together for anastomosis (ensure conduit is inferior)
- Grasp open end with allis clamps x4, then staple across
- Oversew end with vicyrl 2-0 popoffs
- Place crotch stitch with silk 2-0 to reinforce anastomosis and suture inferior mesentery side to prevent internal hernias
Ureteroileal anastomosis
- Incise ureter transversely with tenotomy scissors, then incise proximally to create a T incision
- Line up with conduit, then cut out small window of serosa then mucosa at that site
- Place 4-0 monocryl x2 at base of ureteral incision and attach to conduit, ensure knots are on outside
- Take small ureteral bites (avoid strictures) and suture to conduit
- Once ~75-80% closed, place stent proximally with wire, remove wire to create curl, then grasp with tonsil through conduit and bring out through the stoma, clamp with babcock
- Finish anastomosis, leak test prior to tying knots
Stoma creation
- Grab skin with kocher at marked location, excise a circle of skin and underlying tissue
- Incise fascia in cross-shape, then pass tonsil through incision into abdomen
- Grasp conduit with babock and bring out through stoma site
- Place vicryl stitches x4 through skin, through proximal conduit serosa, then through conduit lip to evert stoma and hold in place, tie down once all 4 placed
- Place extra stitches to secure stoma to skin
- Place nylon suture to secure stents
Closure
- Close midline incision fascia with #1 PDS nonlooped x2, meeting in middle
- Staple skin incisions
- Place ostomy device
Open Cystectomy
Prep and opening
- Male positioning: supine with legs together, place ASIS over break and hyperextend abdomen
- Female positioning: stirrups low lithotomy (cannot hyperextend abdomen)
- Prep in abdomen and genitals, give cefazolin or equivalent antibiotic, have suctions x2, bovie and ligasure
- Make midline incision from L of umbilicus down to pubic symphysis
- Open down to fascia, incise fascia at midline
- Develop space of Retzius, can split endopelvic fascia if able
- Divide urachus superiorly with ligasure, tie with 0 silk stitch on pass to allow for retraction
- Place bookwalter retractor, use short Rich for inferior wall, medium rich for superior wall, and narrow malleable for additional intestinal retraction
Ureteral identification
- Find ureter at bifurcation of common iliacs on either side, if having trouble can identify psoas and track inferiorly
- Isolate ureter with right-angle clamp and vessel loop (tagged), trace inferiorly taking care to maintain periureteral tissue
- Once near bladder, clamp distal ureter with right-angle, cut with Metzenbaum scissors, and tie off stump with 2-0 silk tie
- Cut distal ureteral margin and send for frozen
- Tag lateral edge of ureter (in to out), silk on L side, chromic on R side
- Optional: clip ureters to create iatrogenic dilation in anticipation of anastomosis
Male bladder removal
- Dissect posteriorly to create space between bladder/prostate and rectum
- Ligate pedicles using ligasure, feel below to ensure not on rectum
- Tie off DVC with 0 vicryl on CT-1 in figure-of-8 fashion (x2)
- Clamp urethra prior to removal and tie off with 2-0 vicryl on UR-6
Female bladder removal
- Place sponge stick into vagina to define borders
- Use cautery on 50 to cut through anterior vaginal wall
- Track inferiorly, opening vagina and ligating bladder pedicles
- Tie off DVC with 0 vicryl on CT-1 in figure-of-8 fashion
- Close vaginal opening at midline with 2-0 vicryl in figure-of-8 fashion
- Close lateral vaginal openings with 2-0 V-loc x2, going lateral to medial
Pelvic lymph node dissection
- Identify bifurcation of iliacs
- Take to external iliacs laterally, inguinal ligament distally, and obturator nerve/fossa medially
- Tip: either clip small vessels and cauterize, or use ligasure to prevent lymphocele creation
- Tip: when near the obturator nerve, use metzenbaum scissors instead of cautery
- Place Floseal and fibrillar for hemostasis
Conduit creation
- Pass right-angle under sigmoid mesentery to allow L ureter to pass underneath
- Measure 15cm proximal to ileocecal valve, mark with long silk stitch
- Measure 15-20cm proximal from this mark, mark with short silk stitch
- Create mesenteric window and staple off proximal and distal ends with GIA
- Important step: make sure conduit limb is inferior to planned intestinal anastomosis
- Grasp blind ends and stitch antimesenteric side at base with silk stitch
- Open antimesenteric corner with scissors of each blind end, pass in GIA stapler, and staple together to anastomose
- Grasp open end with allis clamps and use TA stapler to close off, cut off end with scissors
- Oversew the corners and middle with silk stitches
- Close inferior mesenteric window with silk stitch
Ureteroileal anastomosis
- Cut off distal end of bowel with scissors, flush with bulb syringe and drain with pool suction
- Cut bowel serosa with tenotomy, then open mucosa with tenotomy
- Place chromic stitch x3 to evert bowel mucosa
- Cut ureteral end transversely to open, then incise longitudinally to open ureter (insert gerald forceps to dilate)
- Place 4-0 monocryl stitch out/in on ureter and in/out on bowel x2, then tie (make sure tails on same side), then pass one tail around using right-angle clamp and tie together
- Run one stitch up (start on ureteral side) then after 5-6 throws, tie and only cut the loop (tag the tail)
- Place bander stent via distal conduit end, pass out incomplete anastomosis, then feed into ureter and hold in place with Debakeys and remove wire to curl stent
- Run other stitch up, throw x5-6, then tie in same fashion as above
- Use a third monocryl to close the remaining portion of the anastomosis
- Leak test with bulb syringe
- Repeat for other ureter
Ostomy creation
- Cut out skin circle at previously marked location in RLQ
- Find fascia, incise as a lambda and tag the bottom corner with a 2-0 vicryl going out/in (do not cut off needle)
- Putting fingers through main incision and up through ostomy location, cauterize over fingers to open up peritoneum enough for two fingers
- Pass babcock through ostomy incision, bring stents out, then bring out entire conduit, ensure it lays flat inside abdomen
- Place horizontal stitch (using existing 2-0) through proximal intestinal serosa then tie down
- Place 3-0 vicryl stitch (x3) through ostomy opening, proximal serosa (away from mesentery), then through skin, cut and tag, use the other half to place a stitch through just ostomy opening and skin (near mesentery) and tag this too
- Once all stitches placed, tie down and place extra stitches at any visible openings
- Use 4-0 chromic stitch through skin to hold stents together
Closing
- Create window deep to LLQ fascia, make small skin incision and pass through tonsil to place Blake drain into deep pelvis, stitch into place with 2-0 nylon
- Take flex out of bed (if present)
- Close midline incision with 0 PDS looped x2, starting at apex and running towards center
- Every 3-4 stitches, place #2 vicryl as a retention stitch
- Close subQ tissue with 3-0 vicryl and close skin with staples
- Apply ostomy device and dressings
Neobladder (via open approach)
Setting up urethral anastomosis
- Tie off DVC as needed, isolating urethra
- Sharply divide anterior urethra - place double-armed 4-0 monocryl sutures in to out in anterior urethra (clamp with curved hemostat), then place similar sutures in lateral urethra (clamp with straight hemostat)
- Pull foley back and transect urethra completely, place stitches in posterior urethra (clamp with rubbershod hemostat)
Forming neobladder
- Identify ileocecal valve, place silk stitch 10cm proximal, tie with airknot x1
- Subsequently place airknot x2 at 22cm, airknot x3 at 44cm, and airknot x4 at 54cm from original knot (can use vessel loop with staple marked at 22cm at 10cm)
- Create mesenteric windows, staple off proximal and distal ends, then reanastomose intestines superiorly to neobladder segment in normal fashion
- Open distal end of segment, then open antimesenteric intestine with cautery over plastic suction tip (to protect intestine), do not open proximal 10cm (neobladder chimney)
- Designate corners of open intestine: PL and PR for the proximal corners near chimney, DL and DR at the distal open end
- Bring PR and DR together and anastomose with 3-0 vicryl stay stitch, use this to hold traction to place next vicryl stay stitch, continue until posterior edge of neobladder is closed
- Starting inferiorly, run 2-0 V-loc suture along posterior edge until superior edge, maintain tail as a tag for traction
- Neobladder should now be shaped like a U, bring bottom portion of the U up to the anastomosed edges (PR and DR), but offset the bottom towards the right side (away from chimney side)
- Starting at new apex, place 3-0 vicryl interrupted stitches to approximate edges, then calibrate bottom of right side to 24Fr dilator (will use for urethral anastomosis)
- Continue placing vicryls on left side, but do not close completely (will need opening to externalize stents
Ureteral anastomosis
- Anastomose ureters in usual fashion
- Place stent as normal, bring out through open left side of neobladder opening (temporarily)
- Usually do not leak test (difficult to perform)
Neobladder closure and anastomosis
- Place running V-loc starting at R apex and run to superior apex, then continue running to L side
- Before closing, create small opening in neobladder and bring stents through (so that they are not exiting through anastomotic line), tie to neobladder with 4-0 chromic
- Calibrate urethral anastomotic site to 24Fr, place imbricating sutures as needed
- Tag neobladder opening at 3, 6, 9, and 12 o'clock with temporary vicryl stitches, tag with hemostats
- Place posterior stitches (using already placed urethral stitches), re-clamp with rubbershod hemostats
- Place 24Fr Rusch catheter via urethra and insert into neobladder
- Place lateral stitches into neobladder (and clamp), then place anterior stitches - cut out traction stitches as they become no longer required
- Gently bring neobladder down to urethra, then tie starting posteriorly and move anteriorly, inflate balloon
- Create skin incision on L side and bring stents up through incision using tonsil, stitch to skin using 4-0 chromic
Postoperative management
ERAS Postop
- Encourage gum chewing and oral magnesium to avoid ileus
- Consider alvimopan (u opioid antagonist) starting preop
- Start feeding within 4hr after surgery
- Consider epidural for analgesia
- Optimize fluid management and avoid overload
- MgOx daily supplements may help speed up bowel recovery
- Encourage early ambulation
- Extended DVT prophylaxis (apixaban, enoxaparin) recommended x4 weeks after surgery
Neobladder management
- Flushes: start POD#2, usually 30mL BID (small capacity at the start), helps to prevent mucus buildup and clogging
- Mebeverine: antispasmodic agent (not available in US), can decrease risk of undesired bowel contractions, dosed 135mg TID, improved incontinence compared to placebo at 3 months (Hashem 2021)
References
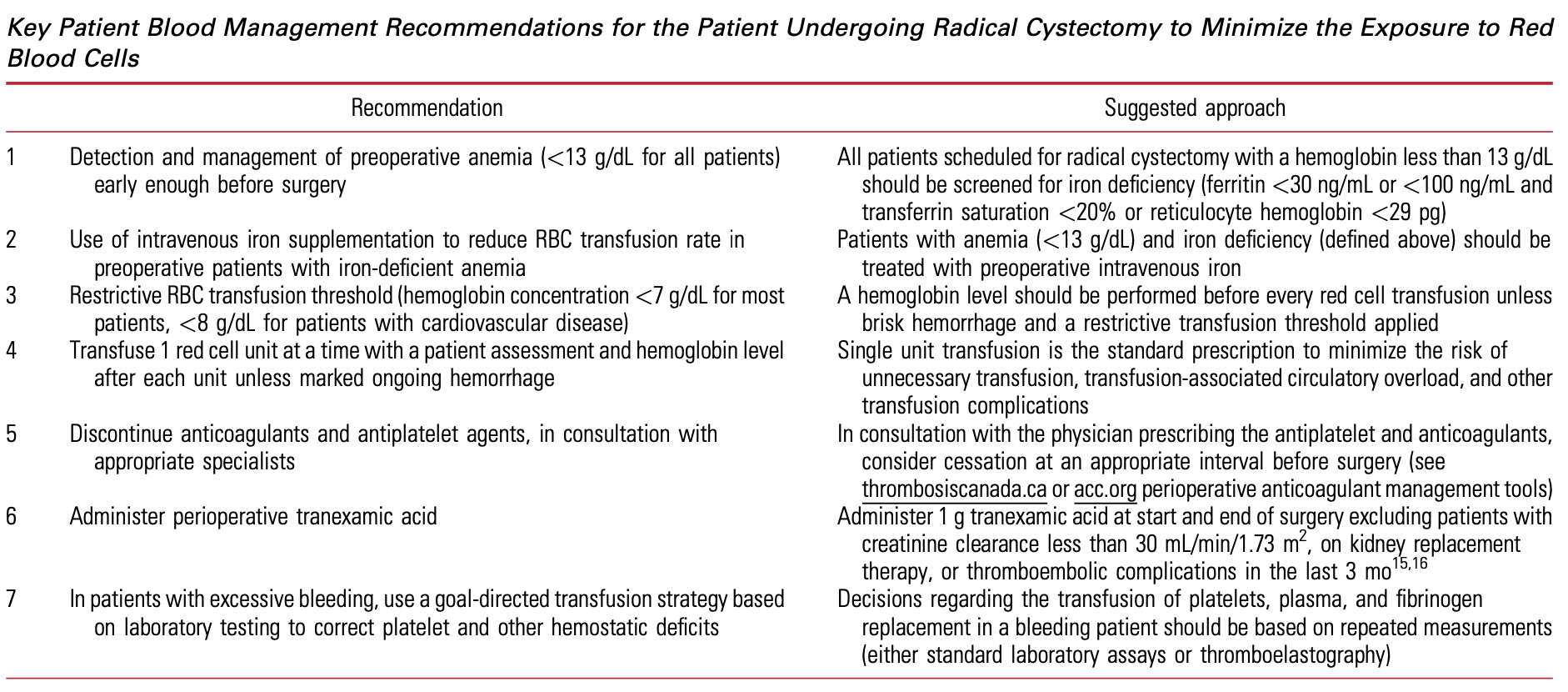
- Callum, Jeannie, and D. Robert Siemens. "We Should Redouble Efforts to Minimize Transfusions in Urological Surgery." The Journal of Urology 209.3 (2023): 471-473.
- Hashem, Abdelwahab, et al. "A Randomized Trial to Examine the Utility of Mebeverine on the Early Return of Continence Following Orthotopic Bladder Substitution." The Journal of Urology 205.5 (2021): 1400-1406.