Stones: Epidemiology and Evaluation
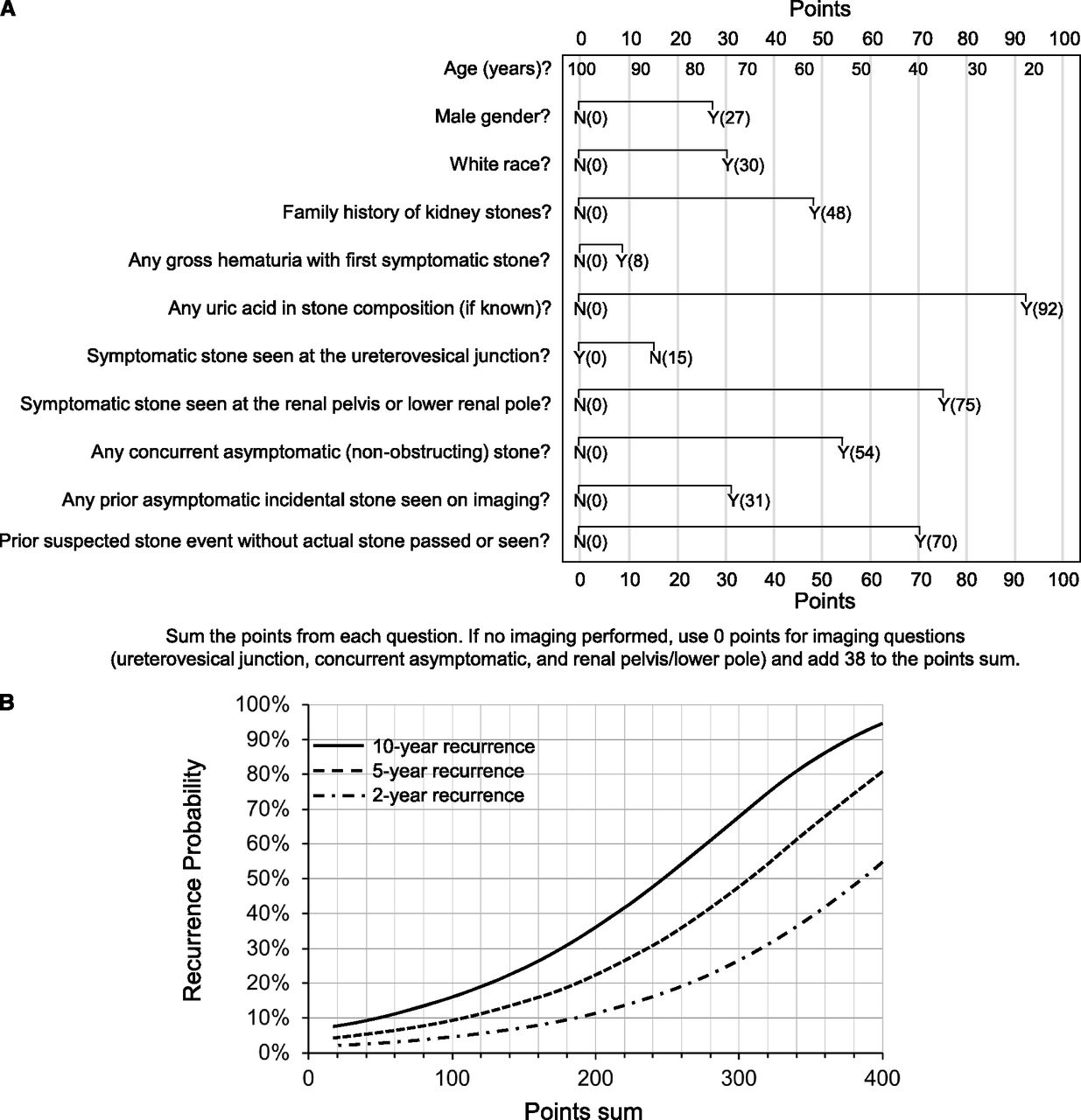
ROKS nomogram for predicting recurrent stone episodes, from Rule 2014
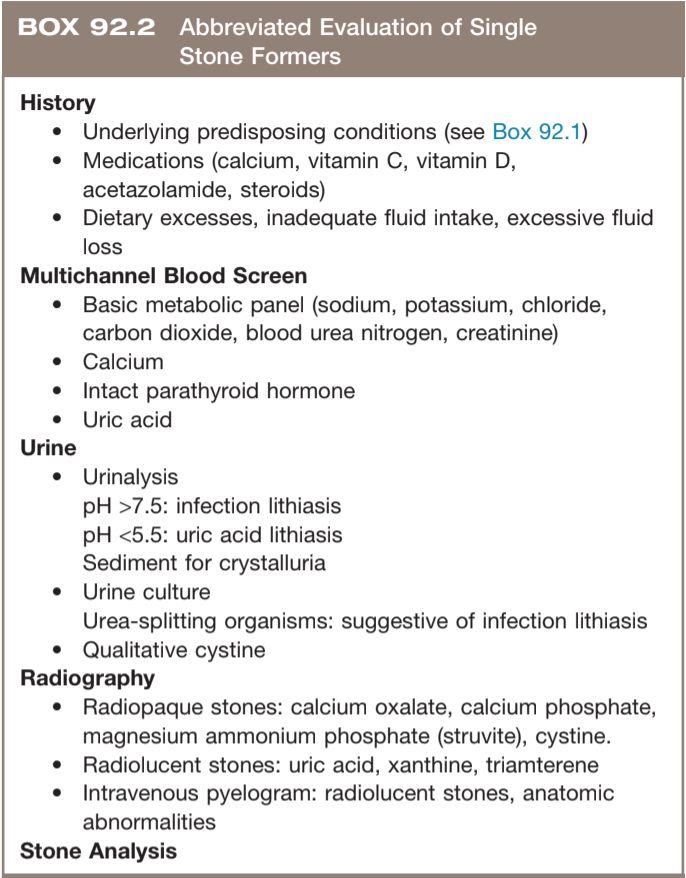
Evaluation after first stone episode, from Campbell's
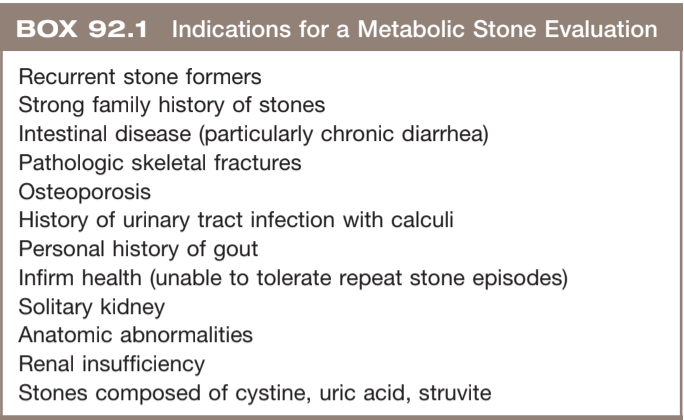
Reasons to get a 24hr urine collection, from Campbell's
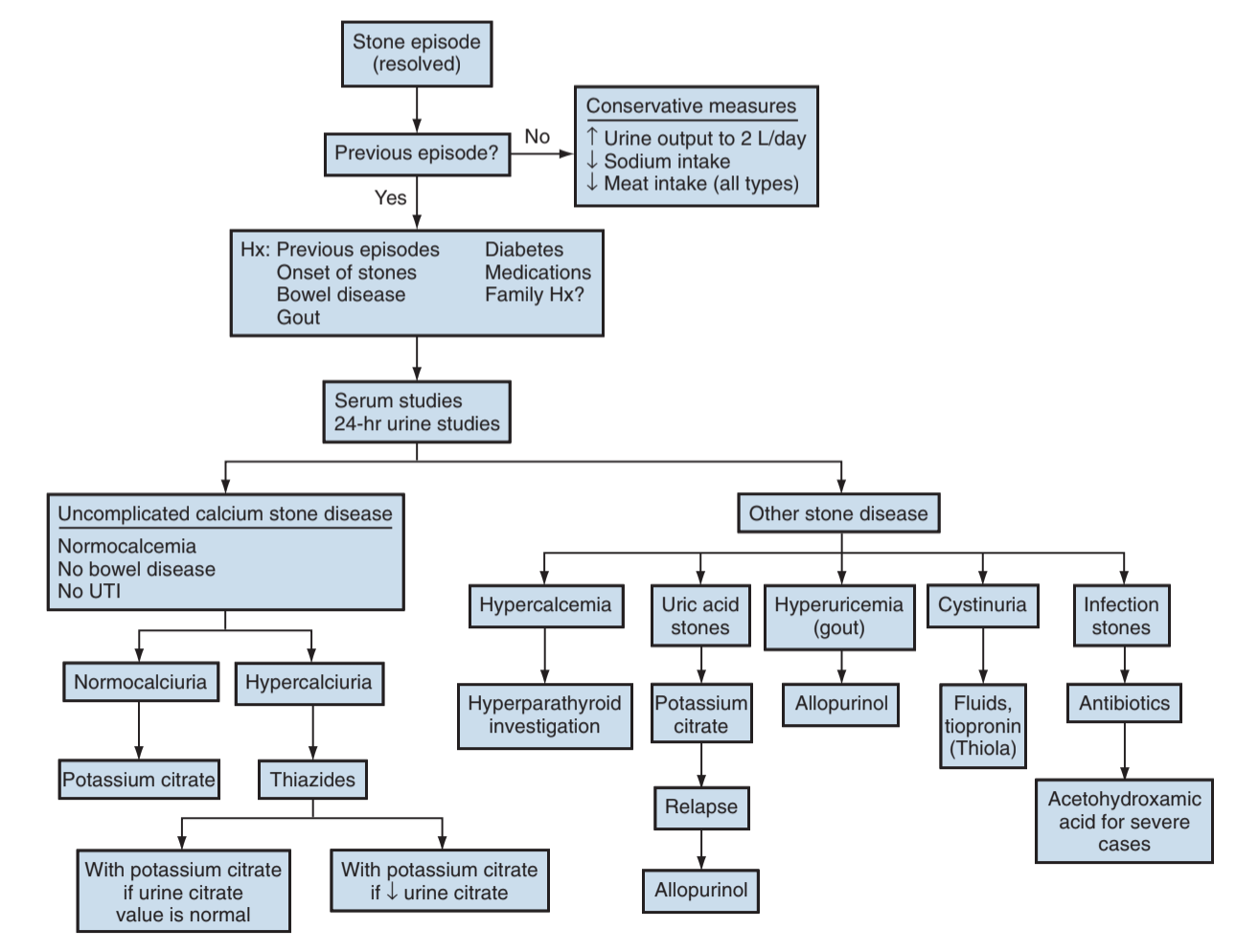
Stone management, from Campbell's
Risk factors
Epidemiology
- Prevalence: 1/11 (9%) people will make a stone (or more) in their lifetimes
- Risk factors: dry/hot climate, obesity, DM (increased uric acid levels, impaired ammonium excretion)
- Recurrence: up to 50% will have another stone episode within 5-10yrs - metabolic syndrome (obesity, HTN, DM) increase stone forming risks
- ROKS nomogram: Created in 2014, predicts risk of stone formation based on patient and stone factors
Factors increasing stone formation
- Calcium: modulated by PTH and Vitamin D, produces both CaOx and CaPhos stones
- Sodium: increased levels get reabsorbed resulting in increased calcium secretion (Na/Ca exchanger)
- Oxalate: component of most common stone type (CaOx), only 20-50% come from diet, vitamin C (absorbic acid) is converted to oxalate
- Uric acid: can act as a nidus for CaOx stone formation, urine levels affected by pH + volume + uric acid quantity, precipitation affected more by urine acidity than uric acid concentration
- Cysteine: disulfide bond results in insolube cystine
Other factors increasing stone risk
- Acidosis: increased urine calcium and phosphate, decreased citrate, increased bone breakdown
- Urease-splitting organsisms: Proteus, Klebsiella, Serratia, Staphylococcus, Morganella, Providencia, Enterobacter
- Matrix: noncrystalline material that forms nidus for stones
Factors decreasing stone formation
- Citrate: main stone inhibitor, complexes with calcium, inhibited by high acid foods (meat, cheese, eggs), fruit/veggies contain the most citrate and have lowest acid load
- Magnesium: complexes with oxalate, inhibits crystal growth
- Phosphate/pyrophosphate: complexes with oxalate, inhibits crystal growth, difficult to increase in urine
- Urea: increases uric acid solubility
- Macromolecules: GAGs (chondroitin and heparin sulfate) and glycoproteins (Tamm-Horsfall and nephrocalcin) inhibit crystal aggregation
Hypercalciuria
- Resorptive: primary hyperPTH increases bone turnover and intestinal absorption, causing hypercalcemia and subsequent hypercalciuria, treated with parathyroidectomy
- Absorptive: increased GI tract absorption of calcium
- Renal: calcium wasting via nephron leakage
- Granulomatous disease: increased 1-alpha hydroxylase (produced by macrophages) -> increased Vitamin D production, treat with steroids
- Thiazide challenge: initiation of thiazide will lead to persistent hyperPTH if primary, but hyperPTH will resolve if secondary
- Overall, no need to differentiate between types besides diagnosing hyperPTH (does not change treatments)
Anatomic risk factors
- UPJ obstruction: assocation questionable, as stone risk persists after treatment of obstruction
- Horseshoe kidney: 20% incidence, thought to be due to high ureteral insertion
- Caliceal diverticulum: combination of urinary stasis and stone forming factors
- Medullary stone kidney: unclear cause, combination of inability to acidify urine, hypercalcuria, hypocitraturia
Medication
- Increase stone risk factors: acetazolamide, topiramate, vitamin C (converted to oxalate), probenacid, antacids, chemotherapy, furosemide
- Directly precipitates as stones: triamterene, guafenesin, ephedrine, indinavir
Types of Stones
- Calcium oxalate: most common type, usually caused by dehydration, difficult to dissolve
- Calcium phosphate: common with hyperPTH, Type 1 RTA, medullary sponge kidney, carbonic anhydrase inhibitor use
- Uric acid: second most common type, usually have normal blood/urine uric acid levels, usually caused by dehydration, radiolucent on KUB, dissolve with alkalinization
- Magnesium ammonium phosphate (struvite): caused by UTI, most common cause of staghorn stones, may dissolve with acidification
- Cystine: seen in cystinuria, may dissolve with alkalinization, positive cyanide-nitroprusside test (urine turns purple if cystine > 75mg/L)
- Ammonium acid urate: seen with laxative abuse and IBD, as well as UTI and hypophosphatemia, may not show up on KUB
- Matrix: seen with UTI, very soft, may not show on imaging
- Indinavir: not seen on non-contrasted CT imaging
Patient evaluation
Patient history risk factors
- Personal/family history stones
- DM/obesity: insulin resistance impairs ammonium excretion, leading to low urine pH and uric acid stones
- Gout: causes hyperuricosuria
- HyperPTH: causes hypercalcemia and hypercalciuria
- Cancer, sarcoid, and granulomatous disease: increases risk for hypercalcemia through PTHrP or Vitamin D
- GI malabsorptions: increase risk for decreased calcium absorption (complexed to fats) and subsequent increased oxalate absorption (normally complexes with calcium and not absorbed)
- Type I RTA: inability to acidify urine from impaired hydrogen secretion in distal tubule, diagnosed with urine pH > 6 and hypokalemia, 75% patients form stones, confirm diagnosis with ammonium chloride loading test (unable to acidify urine after acid load)
- Chronic diarrhea and IBD: causes hyperoxaluria
- Sedentary/immobile: increased calcium absorption and excretion
"High risk" stone formers
- Large stone burden
- 2+ stone episodes
- Nephrocalcinosis
- Pediatric stone formation
- Uncommon stone types: cystine, uric acid, infection (struvite)
- Family history
- Medical conditions with increased risk: gout, IBD, hyperPTH, sarcoidosis, PCKD, RTA, medullary sponge kidney
- Solitary kidney
- Professions with high risk for stone complications
Workup components
- History: medical risk factors (see above), fluid intake, diet, medications, UTI hx
- Blood: electrolytes (BMP), Ca, Phos, Vit D, PTH (if hypercalcemia), uric acid
- UA: assess pH, urine crystals
- Stone analysis: to assess for unusual stone types
24hr Urine Collection
Patient counseling
- Indications for 24hr urine collection: high risk stone formers, abnormal labwork, or desires evaluation
- Timing: wait 1mo after stone treatment and stent removal
- Initial evaluation: obtain 1-2 tests on patient's normal diet
- Repeat evaluation: repeat on stone prevention diet, then start medications if warranted
- Follow-up evaluation: repeat 2-6mo after initial interventions, then consider annual testing
Measured variables
- Volume: < 2-3L/d increases risk for mineral precipitation and stone formation
- Calcium: increased levels (> 200mg/d) lead to increased stone formation, no need to differentiate between the three types
- Oxalate: increased levels (> 40mg/d) complex with calcium and precipitate out, can be due to increased gut absorption
- Sodium: high urinary sodium (> 150mEq/d) leads to decreased proximal tubule sodium resorption causing decreased distal tubule calcium resorption
- Citrate: decreased levels (< 450-550mg/d) result from acidosis and increase calcium stone formation
- Magnesium: can bind oxalate, underlying cause for enteric hyperoxaluria can cause decreased magnesium absorption and subsequent decreased levels (< 80/d)
- Potassium: low levels (< 20-100mg/d)
- Uric Acid: increased levels (> 600-800mg/d) create nidus for CaOx crystallization, but main determinant for precipitation is pH (not uric acid level), abnormally low uric acid + low pH may indicate uric acid stone
- pH: low pH (< 5.5) induces uric acid precipitation, elevated levels increase CaPhos formation
- Sulfate: increased levels indicates high animal protein intake
- Creatinine: indicates adequacy of collection based on expected normal value for creatinine excretion (20-25mg/kg/d for men, 15-20mg/kg/d for women)
- Cystine: normal excretion 0.4% (cystinurics excrete 100%), saturated at 250mg/L, sodium nitroprusside turns purple in presence of cystine, no need to check if initial test normal
Tips for Collection
- Make sure a day is chosen where urine can be completely collected
- Start after first morning void (considered yesterday's urine), and collect until morning void of following day
- Can discontinue Vitamin D, calcium, antacids, diuretics, acetazolamide, and Vitamin C prior to test to assess baseline renal function
References
- AUA Core Curriculum
- Miller, N. L., and M. S. Borofsky. "Evaluation and medical management of urinary lithiasis." Campbell-Walsh Urology. 12th ed. Philadelphia, PA: (2020).
- Pearle, M., J. Antonelli, and Y. Lotan. "Urinary Lithiasis: Etiology, Epidemiology, and Pathogenesis." Campbell-Walsh Urology. 12th ed. Philadelphia, PA: (2020).
- Pearle, Margaret S., et al. "Medical management of kidney stones: AUA guideline." The Journal of urology 192.2 (2014): 316-324.
- Rule, Andrew D., et al. "The ROKS nomogram for predicting a second symptomatic stone episode." Journal of the American Society of Nephrology 25.12 (2014): 2878-2886.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.