Surgical Workup of Kidney Stones
Pre-Surgical Workup
Workup
- Imaging: CT provides stone size, location, and density, better than KUB/US for diagnosis
- Urine culture: obtain preop, patients may have unrelated cystitis that requires treatment
- Anticoagulation: can continue for URS, but stop for PCNL and consider stopping for ESWL
- Isolated pyuria: may be due to stone irritation and may not be due to infection
- Frequency/urgency: can be seen with UVJ stone irritation
- Renal function: consider nephrectomy if stone-containing renal unit has < 15% split function
- HU < 500: likely uric acid, confirm not visible on KUB (if HU equivocal), can trial KCit 20mEq BID or NaBicarb 1300mEq BID
- Treatment indications: ureteral stones > 10mm, failed passage after 4-6wks, causing infection, high-risk professions, patient request
Counseling
- Asymptomatic stones: 50% progression at 5yrs, 15% spontaneous passage, surgical intervention 10-20% within 3-4yrs diagnosis
- Staghorn stones: PCNL is preferred treatment, 50% kidneys with staghorn calculi lose function within 2yrs and 11-30% mortality rate without treatment
- Matrix: ESWL doesn't work, best served with PCNL
- Spontaneous passage of ureteral stones: 71% vs 22% for distal vs proximal, 68% for ≤ 5mm, 47% for 6-10mm
- Timing: treat obstructing stones within 4-6 weeks, otherwise can lead to irreversible renal damage, stones that do not pass within 6 weeks are unlikely to pass (< 5%)
- Need for repeat imaging: per Jackman 2021, patients with persistent ureteral stone often have resolution of pain/hydronephrosis, patients may require repeat CT imaging to confirm passage if stone not collected from urine
Medical expulsive therapy
- Indications: most effective for distal ureteral stones > 5mm, but should be offered if distal stone < 10mm and can be offered for proximal stone < 10mm
- Benefits: 29% increased passage rate, decreased time to passage by 2-4d, decreases pain during passage
Factors complicating surgical planning
Renal stone size affecting surgery choice
- < 1cm: ESWL/URS have equivalent stone free rates
- 1cm-2cm: ESWL affected by stone location (lower pole less efficacious) and size, URS affected by stone size, PCNL not affected by stone size
- > 2cm: PCNL 1st choice, ESWL/URS less efficacious with higher need for secondary procedures
Anatomic considerations
- UPJO: can remove stones at time of repair or perform staged procedure
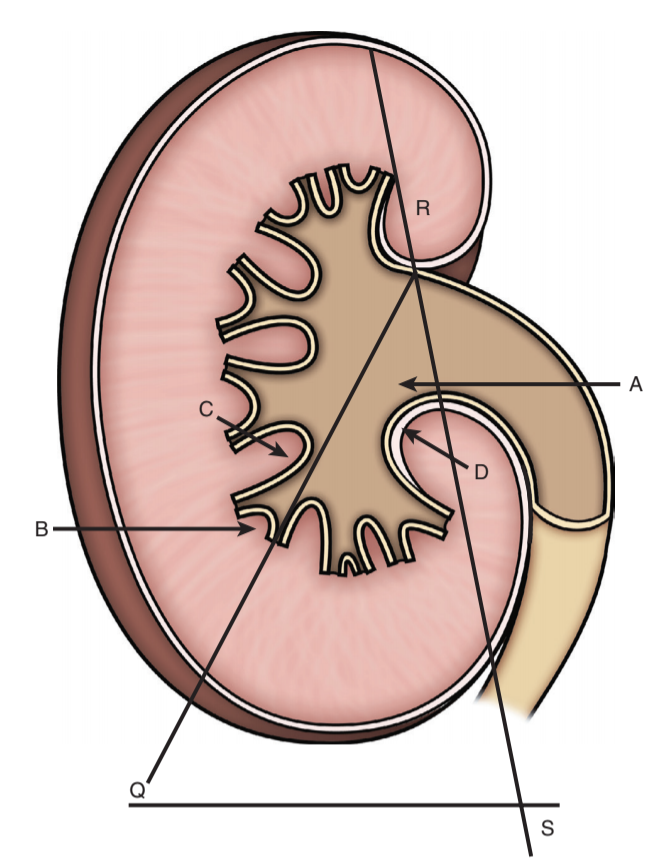
- Calyceal diverticula: rare (0.2-0.6%) and usually asymptomatic, best managed with PCNL
- Horseshoe kidney: 15-20% have kidney stones, can manage based on stone size, ESWL usually less effective due to more complex drainage
- Pelvic kidney: can consider any treatment option, large stones require PCNL or even laparoscopic removal
- Duplicated ureter: uncommon (0.8%), consider retrograde pyelogram
- Ureteral stricture: consider stenting or balloon dilation
- Solitary kidney: consider prophylactic treatment of asymptomatic stones
- Urinary diversion: antegrade approach usually best, PCNL stone free rates 75-88%
- Transplant kidney: prophylactic treatment recommended as lack of innervation will lead to lack of presenting obstructing symptoms
Lower pole location complicates surgeries
- Surgical choice: mainly affects ESWL planning, no effect on PCNL (may be easier), improving URS technology is decreasing issues with lower pole stone treatment
- Imaging findings: assess infundibulopelvic angle, infundibular length, infundibular width
- Dust vs fragment: less likely to spontaneously pass after fragmentation
Emergent Drainage
Criteria for emergent/urgent stent/PCN
- Evidence of infection: fever, leukocytosis, UA with bacteria/WBC
- All renal units blocked: bilateral stones, or unilateral stone in solitary kidney
- Uncontrolled pain/nausea: patient unable to remain home on PO meds
- Hydronephrosis: prolonged or severe unilateral obstruction
Should a patient undergo PCN or stent?
- Pearle 1998: only RCT in literature, no difference in outcomes
- PCN benefits: higher spontaneous stone passage rate, no anatomic restrictions (stricture, finding UO), patients report better pain tolerance, don't actually mind bag as much, better drainage with larger/multiple stones
- Stent benefits: no need to hold anticoagulation
- Bottom line: PCN outperforms stent in all parameters (including patient satisfaction), but stent should usually be attempted if IR is unwilling or unable
Follow-Up
After surgery
- Labs: can obtain 24hr urine once surgery completed and stent/PCN removed
- Imaging: postoperative ureteral obstruction with silent hydronephrosis occurs in ~2% (1/50 in the original study), renal US 4-6 weeks after stent removal recommended for all patients, also obtain KUB to rule out residual fragments
- Residual fragment management: fragments > 4mm have high risk of further growth (30-40% will grow by 3-6yr), pain, and requiring additional treatments (10-30%), higher risk with infection stones, should offer repeat PCNL/URS, however US does overestimate stone size (Ganesan 2017)
Long-term
- Labs: repeat 24hr urine 6mo after initial assessment to check for improvements, then consider checking on annual basis to assess for adherence
- Imaging: no clear evidence for long term screening, minimal data for annual KUB + renal US to assess for stone formation/growth
References
- AUA Core Curriculum
- AUA Guidelines: Surgical Stone Management
- Fedrigon, Donald, et al. "SKOPE—Study of Ketorolac vs Opioid for Pain after Endoscopy: a double-blinded randomized control trial in patients undergoing ureteroscopy." The Journal of urology 206.2 (2021): 373-381.
- Fulgham, Pat Fox, et al. "Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment." The Journal of urology 189.4 (2013): 1203-1213.
- Ganesan, Vishnu, et al. "Accuracy of ultrasonography for renal stone detection and size determination: is it good enough for management decisions?." BJU international 119.3 (2017): 464-469.
- Hiller, Spencer C., et al. "Ureteral stent placement following ureteroscopy increases emergency department visits in a statewide surgical collaborative." The Journal of urology 205.6 (2021): 1710-1717.
- Jackman, Stephen V., et al. "Resolution of Hydronephrosis and Pain to Predict Stone Passage for Patients With Acute Renal Colic." Urology 159 (2022): 48-52.
- Leavitt, D., J. de la Rosette, and D. Hoenig. "Strategies for Nonmedical Management of Upper Urinary Tract Calculi." Campbell-Walsh Urology. 12th ed. Philadelphia, PA: (2020).
- Matlaga, B. and A. Krambeck. "Surgical Management for Upper Urinary Tract Calculi." Campbell-Walsh Urology. 12th ed. Philadelphia, PA: (2020).
- Pearle, Margaret S., et al. "Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi." The Journal of urology 160.4 (1998): 1260-1264.
- Sur, Roger L., et al. "A randomized controlled trial of preoperative prophylactic antibiotics for percutaneous nephrolithotomy in moderate to high infectious risk population: a report from the EDGE consortium." The Journal of urology 205.5 (2021): 1379-1386.
- Tapiero, Shlomi, et al. "Determining the safety threshold for the passage of a ureteral access sheath in clinical practice using a purpose-built force sensor." The Journal of urology 206.2 (2021): 364-372.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.