Urologic Care for Transgender Patients

Terms to use for transgender and other LGBTQ+ patients, from Campbell's
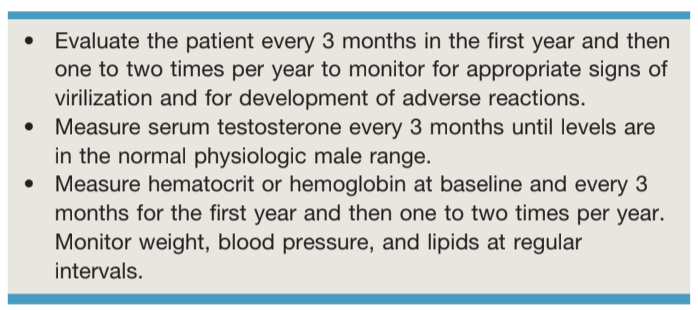
Follow up after starting testosterone, from Campbell's
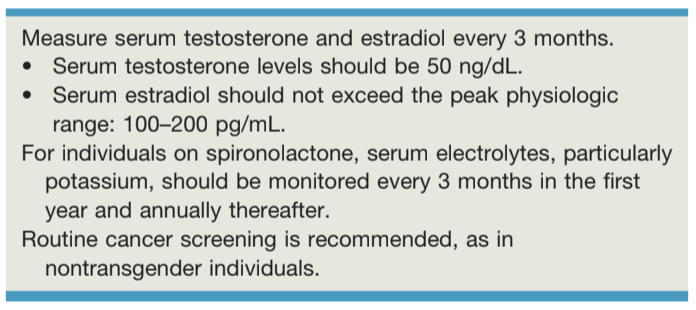
Follow up after starting estrogen, from Campbell's
Transgender Patient Care
Assessment of overall health
- Steps towards transition: cross-dressing, hormonal therapy, gender-affirming surgery
- Physical exam to assess secondary sex characteristics
- Consider topical estrogen for 1-2 weeks prior to a pelvic exam
- DO NOT perform genital exam unless clearly indicated
- IMPORTANT: establish trust and decrease anxiety, just as for any patient
Fertility
- Treatments may have permanent effects on fertility, discuss side effects and goals prior to initiating irreversible treatments
- Sperm may need to be obtained through electroejaculation or extraction after treatments
MTF hormone therapy
- Goals: administer estrogens (goal < 200pg/mL) with antiandrogen medications - 5ARi or spironolactone, aim for testosterone 30-100ng/dL
- Side effects: estrogen increases cardiac, cerebrovascular, breast cancer, and hyperlipidemia risks
- Prostate cancer: rare in patients with supressed testosterone, can monitor PSA, consider that DRE may enhance gender dysphoria
FTM hormone therapy
- Goals: can administer testosterone alone, aim for 300-1000ng/dL
- Side effects: testosterone increases polycythemia, liver dysfunction, cardiac, cerebrovascular, and hypertension risks
- Ovarian concerns: testosterone does not seem to cause PCOS or affect the potential follicle reserve
Gender-Affirming Surgeries
Transgender Woman Surgeries
- Creating vaginal cavity between bladder and rectum puts nerve supply to sphincter and bladder at risk
- Prostate not removed, potential risk for prostatic pathologies, use PSA cutoff 1.0, can be assessed on neovaginal exam (instead of DRE)
- Leave urethral catheter for 10 days, then assess voiding function
- Vaginoplasty/vulvoplasty: disassemble corpora, create perineal urethrostomy, define space between bladder/rectum, create vagina from skin/intestine, perform clitoroplasty and labiaplasty
- Clitoroplasty: keep portion of glans attached to neurovascular bundle to allow for sensate neoclitoris
- Labiaplasty: use scrotal skin to create labia majora
- Vaginoplasty maintenance: lifelong dilation, lubrication, and hygiene
- Can perform vulvaplasty to provide appearance without vaginal canal
- Orchiectomy: allows patient to stop antiandrogens and decrease estrogen dose (less side effects), easier to "tuck"
- Complications: abnormal urinary stream (33%), urethral stenosis (15%), vaginal stenosis (10%)
Transgender Man Surgeries
- Potential goals: gender-congruent genital appearance, standing to void, ability to have intercourse
- Surgical goals: remove female anatomic structures, create normal male anatomic structures, and implant penile/testicular implants
- Surgery specific workup: manage LUTS, assess PVR, and renal US to rule out upper tract pathologies
- Remove complete uterus, cervix, and tip of vagina
- Vaginectomy: unclear when is best timing (staged vs all-in-one), not required for phalloplasty
- Urethroplasty: use vestibular mucosa to create "bulbar" urethra, clitoris fixed to pubic symphysis to provide continued sensation, bulbospongiosus muscles closed over urethra to prevent fistulas and postvoid dribbling
- Phalloplasty: tube-within-a-tube created from radial forearm or thigh flap
- Scrotoplasty: created from labia majora, flaps supplied by external pudendal artery
- Metoidioplasty: alternative to phalloplasty, enlarges clitoris without creating an organ adequate for penetrative intercourse, buccal mucosa graft may be necessary to create short tubular urethra
- Testicular prosthesis: implant 6mo after scrotoplasty, fix into pouch to prevent migration
- implant 12mo after phalloplasty if no urethral issues and sensation intact, can implant single-cylinder IPP, can fix to pubic bone periosteum, erosion/infection rate 20%, replacement rate 44%
- implant 12mo after phalloplasty if no urethral issues and sensation intact, can implant single-cylinder IPP, can fix to pubic bone periosteum, erosion/infection rate 20%, replacement rate 44%
- Catheter: place urethral and SPT, can remove urethral catheter after 12 days, remove SPT once voiding is normal
- Catheterization: use Tiemann (stiff Coude) to pass sharp urethral angle x1, otherwise use cystoscopy
- Urethral complications: overall 40%, fistula (15-70%), stricture (25-58%), postvoid dribbling common (provide perineal pressure to empty), flap loss (1%)
References
- AUA Core Curriculum
- Elsamra, S. "Evaluation of the Urologic Patient: History and Physical Examination." Campbell-Walsh Urology 12 (2020).
- Kocjancic, E., V. Iacoveilli, and O. Acar. "Sexual Function and Dysfunction in the Female." Campbell-Walsh Urology 12 (2020).
- Lumen, N., A. Spinoit, and P. Hoebeke. "Special Urologic Considerations in Transgender Patients." Campbell-Walsh Urology 12 (2020).