Male Infertility Evaluation
Normal Physiology
Normal sperm development
- Spermatogenesis: occurs in spermatic tubules, mitosis (spermatogonia to spermatocytes), meiosis x2 (primary spermatocytes to secondary spermatocytes to spermatids), spermiogenesis (spermatids to spermatozoa)
- Maturation: occurs in epididymis, acquire mobility and capacity to fertilize, completed at epididymal tail (stored here)
- Capacitation: activation of sperm's ability to fertilize egg, only occurs in female genital tract
- Hypermobility: increased mobility occurs after capacitation (only in female genital tract)
- Acrosome reaction: head of sperm releases enzymes to dissolve the outer layer of ovum
Normal male ejaculation
- Controlled by spinal ejaculatory center (T12-L2)
- Emission: sympathetic mediated, bladder neck contraction, release of fluid into posterior urethra (stimulates urethral-muscle reflex)
- Expulsion: activated by urethral-muscle reflex, contraction of bulbospongiosus/ischiocavernosus, mediated by pudendal nerve
Infertility Workup
Timing
- Wait 1yr before starting workup, 6mo if woman > 35yo
- 75% can achieve pregnancy within 6mo trying, 85% within 12mo, 90% within 2yr
- 30% male infertility will be identified as idiopathic
- Both partners need to undergo workup
- Consider if 2+ pregnancy losses or failed artificial reproduction cycles
History
- Prior pregnancies and childbirth: some men may have had prior children
- Ejaculate frequency: semen parameters peak after 1-2 days, then decline - no benefit in abstaining for long periods to "build up" semen
- Intercourse: timing, frequency
- Comorbidities: higher risk of infertility with HTN, HLD, obesity, DM, hypo/hyperthyroidism
- No association with infertility: caffeine, cell phones
Medical Causes
- TICS: Toxins, Infections/inflammation, Childhood history, Sexual history
- Neurologic: DM, SCI, and MS all affect normal ejaculation
- Cancer: can negatively affect sperm parameters even prior to treatment, testis cancer has even greater effect
- Hyperthermia: cryptorchidism, heated seats, and laptop heat should be avoided
- Infections: can cause strictures, prostatitis, testis failure, pre-pubertal mumps does not affect fertility, wait 3mo after febrile illness to check semenalysis
- Medical risk factors: liver failure, DM, thyroid disorders
- Hydrocele: increased prevalence in infertile patients but unclear cause and unclear benefit to performing hydrocelectomy
- Kartagener syndrome: nonmotile cilia prevent sperm motility, also have bronchiectasis, sinusitis, situs inversus, diagnose with evaluation of axoneme
- Young syndrome: thick epididymal secretions obstruct the vas, may also have bronchiectasis and sinusitis
- Cystic fibrosis: absent vas, bronchiectasis, sinusitis, pancreatic disease, evaluate with CFTR panel
- Congenital bilateral absence of vas deferens (CBAVD): isolated absence of vas (no URI symptoms)
Surgical Causes
- RPLND: results in retrograde ejaculation
- Hernia repair: can obstruct vas deferens or testicular blood supply, 1-2% vs 0.3% pediatric vs adult repair
- Pediatric inguinal surgery: testis atrophy develops in 0.3%
- Torsion: oligospermia (36-39%), antisperm antibodies (11%)
- Cryptorchidism: paternity rates 96% (unilateral) and 70% (bilateral), orchiopexy recommended before 10yo
Medication Causes
- Endocrine modulators: antiandrogens, spironolactone, HAART, steroids, estrogens, cimetidine, finasteride, allopurinol
- 5ARi: questionable effect on semen parameters, can consider stopping
- Anabolic steroids: inhibits LH, withdrawal can take months/years to reverse
- Illicit drugs: marijuana may decrease tesosterone, alcohol converts T to E, tobacco may affect sperm parameters, cocaine has questionable effects
- Antipsychotics: antidopamine effect leads to elevated prolactin
- Opioids: suppress LH at the hypothalamic level
- Chemotherapy: can lead to DNA damage at 2yrs after administration, mainly platinum-based, alkylating agents, antimetabolites, vinca alkaloids, topoisomerase inhibitors
- Antibiotics: tetracycline can be directly spermatotoxic, nitrofurantoin may have negative temporary effect
- Sulfasalazine: leads to oligoasthenospermai, can switch to mesalazine
- Environmental/Occupational exposure: heavy metals, pesticides, hyperthermia
Physical Exam
- Secondary sexual characteristics: pubic hair, gynecomastia, arm span > 5cm height
- Obesity: increased aromatase conversion to estradiol
- Genital exam: location/size of testes, presence of varicocele, palpable vas deferens, abnormal urethral appearance
- DRE: optional, SVs not normally palpable
Lab Evaluation
Semenalysis
- Highly variable, check minimum 2 separated by 2-4 weeks
- Abstain from ejaculation for 24hrs (not more) to provide optimal sample
- Volume: consider workup if < 1.0-1.5mL
- Density: oligospermia (< 13.5million/mL) and cryptozoospermia (so few it's hard to measure)
- Total #: volume x density (normal > 39mil)
- Motility: asthenospermia (normal > 32%)
- Morphology: teratospermia (overabundance of abnormal forms), globospermia (lacking acrosomes) normal > 4%
- Vitality: necrospermia (large number nonliving sperm), normal > 58%
- Antisperm antibodies: due to injury of blood/testis barrier, suspect if sperm agglutination or decreased motility, seen in vasectomy, testis trauma, orchitis, cryptorchidism, testis cancer, varicocele
- Pyospermia: > 1million/mL, may cause injury secondary to reactive oxygen species, Pap smear will differentiate WBCs from immature germ cells
- Fructose level: > 13umol/ejaculate, low levels may indicated ejaculatory duct obstruction
Hormonal labs
- Indications: not required for every patient, obtain if concern for impaired libido, erectile dysfunction, oligozoospermia, azoospermia, atrophic testes, or abnormal physical exam
- Testosterone: normal > 280-300, 55+% should be bioavailable (check albumin + SHBG), peaks in the morning
- LH/FSH: sertoli dysfunction indicated by elevated FSH, testicular dysfunction indicated by elevated LH
- Estrogen: T/E ratio < 10 may indicate testicular dysfunction
- Prolactin: consider testing if infertility associated with visual field changes, headaches, or ED, repeat if elevated level (large variation)
- Inhibin-B and Anti-Mullerian Hormone: can assess Sertoli cell function
- 17OH-progesterone marker for intratesticular testosterone level, nonexistent if patient using exogenous T
- Hypergonadotropic hypogonadism: elevated LH/FSH with low T, indicates testicular dysfunction
- Hypogonadotropic hypogonadism: low LH/FSH/T, indicates pituitary dysfunction
- Solitary testis: may demonstrate normal semen parameters and testosterone level but relatively higher level of FSH/LH than would be considered normal due to pituitary response
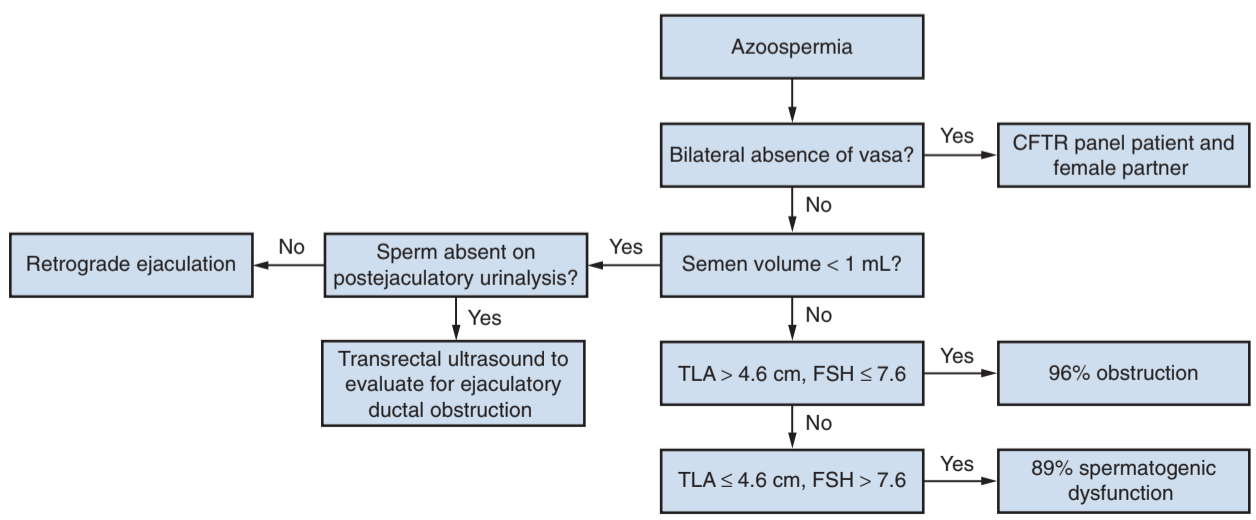
Azoospermia
- Obstructive: likely cause in 96% of patients with FSH < 7.6 and testis > 4.6cm
- Nonobstructive: likely cause in 89% of patients with FSH > 7.6 and testis < 4.6cm
- Biopsy: not indicated for initial workup, consider if indeterminate findings
References
- AUA Core Curriculum
- Niederberger, C., S. Ohlander, and R. Pagani. "Male Infertility." Campbell-Walsh Urology 12 (2020).
- Schlegel, Peter N., et al. "Diagnosis and Treatment of Infertility in Men: AUA/ASRM Guideline." (2020).
- Tradewell, Michael B., et al. "Evaluation of reproductive parameters in men with solitary testis." The Journal of urology 205.4 (2021): 1153-1158.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.