Erectile Dysfunction
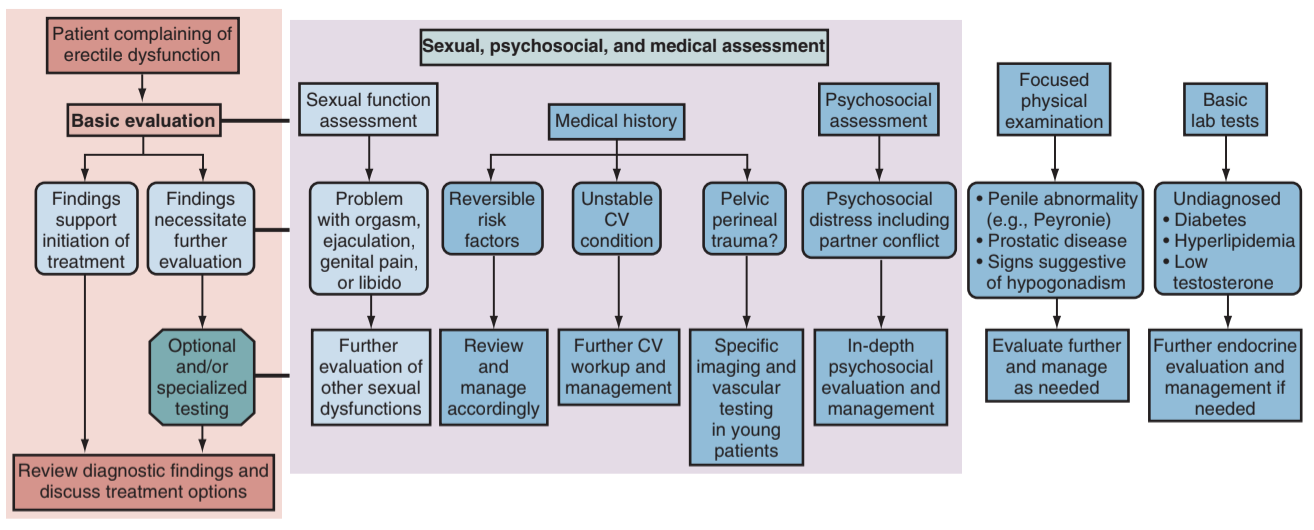
Eval/Workup
History
- HPI: onset, severity/rigidity, degree of bother, situational factors, pain, stable/worsening symptoms
- Age: prevalence 1-10% < 40yo, 15% 40-49yo, 30% 50-59yo, 40% 60-69yo, 50-100% 70-90yo
- Commonly associated risk factors: HTN (38-42%), DM (20%), HLD (42%), depression (11%), premature ejaculation (30-60%)
- PMHx: cardiovascular disease, DM, endocrine issues (hypoT), neurologic disorders, psych diagnoses (depression, anxiety, stress), liver disease, alcoholism
- PSHx: prostatectomy, cystectomy, aortoiliac vascualr surgery, aneurysm repair, proctocolectomy, pituitary surgery, penile surgery, pelvic trauma
- Meds: antiHTN, SSRIs, TCAs, antipsychotics, MAOi, antiandrogens, cimetidine, opiates, 5ARi, LHRH agonists/antagonists, prior ED therapies
- Social Hx: partner(s), substance use
- Psychosexual factors: social, cultural, religious, education
Key Questions
- Are you able to obtain + sustain an erection satisfactory for intercourse?
- Do you have morning and/or nocturnal erections?
- Are you able to masturbate?
Physical
- Vitals: check for uncontrolled HTN
- Testosterone deficiency: obesity, gynecomastia, decreased body hair
- Genital exam: hypogonadism, penile curvature, testis presence and size
- DRE: not required for evaluation
Further Diagnostics
- Questionnaires: IIEF or SHIM (abridged version of IIEF)
- Labs: can check BMP, glucose, lipids, HbA1c, testosterone (draw in AM)
- Low testosterone: check bioavailable (serum-free) T (albumin + SHBG) and luteinizing hormone, consider prolactin and estrogen
- Further workup (see below): consider if young, family hx cardiac disease, pelvic trauma, failed prior therapy, likely psychogenic, Peyronie disease, lifelong ED
Adjunct testing
- Almost never required prior to offering treatment options, as only patients with arterial insufficiency benefit from specific treatment options
- Nocturnal penile tumescence/rigidity (NPTR): detects erections during REM w/ strain gauge, BP cuff, "stamp roll test," determines organic vs psychogenic ED
- ICI + stimulation: good erection after 10min rules out veno-occlusive disease but not arterial insufficiency
- Penile duplex doppler sonography: perform ICI then examine, check arterial and venous flow
- Cavernosometry: place two needles in corpora, infuse heparinized saline and inject erectogenic medication, measure intracavernosal pressure, assess "flow to maintain" (flow required to maintain pressure 150mmHg) and "intracavernosal pressure decay (pressure decline after stopping infusion)
- Cavernosography: infuse contrast during cavernosometry and obtain images
- Pudendal arteriography: gold standard for assessing arterial insufficiency, assess patency of inferior epigastrics, stenosis of penile blood supply, ability to bypass blockages
- Cavernous arterial systolic occulsion pressure (CASOP): perform ICI, then use BP cuff to determine presure when blood flow becomes detectable
- Penile brachial index: similar to CASOP but measured when flaccid, penile SBP divided by brachial SBP
| Test | Arterial insufficiency | Venous leak | Psychogenic ED |
|---|---|---|---|
| NPTR | Poor erection | Good erection | |
| ICI + stimulation | |||
| Penile ultrasound | PSV < 30cm/s PSV < 60cm/s (sum of R + L) cavernous artery diameter < 0.7mm |
Normal PSV, EDV < 3cm/s RI ≤ 0.8 |
No abnormalities |
| Cavernosometry | No abnormalities | Flow to maintain < 3mL/min IC pressure decay > 45mmHg in 30s |
|
| Cavernosography | Venous drainage visualized | ||
| CASOP | Brachial SBP - CASOP < 35mmHg | No abnormalities | |
| Penile brachial index | PBI ≤ 0.7 | ||
Cardiac evaluation
Importance of evaluation
- Penis/heart relationship: the penis is the dipstick of the heart, development of ED can predate cardiac disease by 5-10 years (25% increased risk at 10yrs)
- MI risk during intercourse: sex causes < 1% MI, absolute risk < 0.01% within 2hr sex
- Assess METS: ask whether patient tolerate 20min walking on flat surface or walking 2 flights stairs in 10 seconds, if patient can tolerate 3 METs activity without chest pain then can tolerate sexual activity
- Workup: check blood pressure, T, lipids, HbA1c if not checked within past 12mo
- Cardiac meds: PDE5i contraindicated if taking nitrates, guanylate cyclase stimulators (riociguat, nicorandil), vardenafil contraindicated with QT prolonging antiarrhymthics, a-blockers + PDE5i can worsen hypotension
Princeton III criteria
- Low risk: no cardiac disease and able to exercise w/o symptoms, have undergone successful revascularization, Class I-II heart failure, controlled asymptomatic HTN, mild cardiac valve disease
- Intermediate risk: mild/moderate stable angina, MI in past 2-8 weeks, Class III heart failure, or non-cardiac vascular disease (PVD, CVA, TIA)
- High risk: unstable/refractory angina, recent MI (< 2 weeks), arrythmias, uncontrolled HTN/DM, Class IV heart failure, moderate/severe valve disease, obstructive hypertrophic cardiomyopathy
- Management: intermediate/high risk require cardiology consult/evaluation prior to starting ED therapies, low risk requires no further workup
PDE5 Inhibitors
Tips for Improved Efficacy
- Use 9-10 times before increasing dose
- Increased dose increases side effects but not efficacy
- Sexual stimulation required
- No evidence that early use helps regain erections after prostatectomy
- Overall 70% report success with sexual intercourse, only 40-50% if diabetic
Risks/Contraindications
- Contraindications: nitrates, severe liver/renal disease
- Relative contraindications: baseline hypotension or hypertension, drugs that increase PDE5i halflife (Cyp-P450 3A4 inhibitors), retinitis pigmentosa, cardiovascular disease
- a-blockers + PDE5i: okay to use but increased risk for hypotension
- nitrates + PDE5i: no pharmacologic antidote if co-administered
- Hypotension management: fluids, a-agonists, Trendelenburg position, rarely requires intraaortic balloon pump
- Cross-reactions: antidepressants, antifungals, antiHTN, HAART
- Common side effects: dyspepsia (4-10%), headache (7-16%), flushing (4-10%), myalgia + back pain (0-3%, congestion (3-4%), visual disturbances (0-3%)
- Blue/green color vision change: due to PDE6 cross-reactivity, not seen with tadalafil
- Sudden unilateral vision loss (NAION): overall extremely rare (3/100K), possibly not even a real association
Options
| Drug | Dosing | Onset | Avoid with fatty food | Headache/Dyspepsia/Flushing | Backache/Myalgias | Blurred/Blue Vision |
|---|---|---|---|---|---|---|
| Sildenafil (Viagra) | 25-100mg | 30-60min | Yes | Yes | Rare | Yes |
| Tadalafil (Cialis) | 5-20mg | 60-120min | No | Yes | Yes | Rare |
| Vardenafil (Levitra) | 5-20mg | 30-60min | Yes | Yes | Rare | Rare |
Everything but PDE5i and IPP
Lifestyle changes
- General tips: maintain ideal weight, exercise
- Drug use: stop smoking, alcohol, and other drug use
- Medications: stop or switch to medications with lower ED risk
- Comorbidities: optimize HTN, DM, cardiac disease
- Psychogenic ED: consider sexual counseling
Intracavernosal Injections
- Options: alprostadil (cAMP stimulator), papaverine (non-specific PDEi), phentolamine (a1-blocker), atropine, bimix (papaverine + phentolamine), trimix (bimix + alprostadil)
- Efficacy: 54-100%, satisfaction 46-99%
- Side effects: priapism (highest with papaverine), pain (highest with alprostadil), fibrosis (highest with papaverine), hypotension and systemic side effects (highest with veno-occlusive leak)
- Contraindications: hx pripaism, coagulopathy, unstable cardiac disease, reduced manual dexterity, MAOi use (HTN crisis if a-agonist needed to reverse a priapism)
- Anticoagulation: not a contraindication, hold pressure to prevent hematoma
- Dosing: alprostadil (2.5-60ug/mL), bimix (20ug/mL + 0.5mg/mL), trimix (10ug/mL + 30mg/mL + 1mg/mL), maximum 3x weekly with > 24hr between doses
Vacuum Assist Device + Occlusion ring
- Satisfaction: patient (60-80%), partner (70+%)
- Weak seal: trim pubic hair and use adequate lubricant
- Abnormal sensation: may create fulcrum effect (flaccid proximal, rigid distal) or abnormal feel/appearance (blue/gray color, cool to touch)
- Side effects: bruising (18%), pain (18%), difficult ejaculation (22%), device difficulty (20%)
- Contraindications: priapism risk, penile fibrosis, bleeding disorder or anticoagulation (can cause hematoma)
- Frequency: do not use for > 30min, wait at least 1hr between uses
Intraurethral Alprostadil (MUSE)
- Dosing: 125, 250, 500, 1000 mcg
- Directions: urinate before use, insert pill/applicator, roll penis to dissolve medication, use maximum BID, test in office prior to prescribing (2% risk hypotension)
- Efficacy: 50-70%
- Side effects: genital pain (6.5-35%), urethral trauma (1-5%), urethral pain (0-29%), dizziness (0-7%), painful erection (1%), potential risk for priapism
- Contraindications: high risk for priapism, distal urethral stricture, penile fibrosis, balanitis, urethritis, having sex with pregnant woman (unless using condom)
Testosterone therapy (see separate page)
- Do not supplement testosterone if normal T levels
- Baseline assessment: DRE, PSA, CBC, LFT, lipids, repeat 3-6mo after starting treatment, then annually
- Give short course testosterone (3mo), if no improvement then discontinue
- Common side effects: increased Hgb, OSA, gynecomastia, acne
Arterial revascularization
- Indications: only patients with proven arterial insufficiency, usually focal stenosis from trauma
- Contraindications: atherosclerosis, veno-occlusive disease, tobacco use
- Procedure: anastomose inferior epigastric to dorsal penile artery or deep dorsal penile vein, can cause glans hyperemia, success rates 60-70% at 5yr
Penile Prosthesis
See separate page for counseling, techniques, and postoperative troubleshooting
References
- AUA Core Curriculum
- Burnett, A. and R. Ramasamy. "Evaluation and Management of Erectile Dysfunction." Campbell-Walsh Urology 12 (2020).
- Burnett, Arthur L., et al. "Erectile dysfunction: AUA guideline." The Journal of urology 200.3 (2018): 633-641.
- Mellon, M. and J. Mulcahy. "Surgery for Erectile Dysfunction." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.