Upper Tract Obstruction
Workup
What happens during upper tract obstruction?
- Phase 1 (1-2hr): ureteral pressure and RBF increase, afferent arteriole vasodilates to offset drop in GFR (drops 50% in 4hr, 75% in 12hr, 95% in 24hr)
- Phase 2 (3-4hr): ureteral pressure rises but RBF decreases
- Phase 3 (5+hr): ureteral pressure and RBF decrease due to afferent arteriole vasoconstriction, RBF drops to 70% at 24hr, 50% at 72hr, 20% at 2wks, and 12% at 8wks
- Bilateral obstruction: RBF increases slightly for 90min, then RBF and medullary blood flow decline, ureteral pressure remains elevated x24hr
Initial evaluation
- Symptoms: flank pain/fullness, often asymptomatic if chronic
- Dietl's crisis: pain with increased fluid intake (specific not sensitive)
- History vesicoureteral reflux (may cause ureteral dilation and kinking)
- History stones (especially impacted), stone surgery (URS stricture rate < 1%)
- History malignancy, XRT
- History AAA or endometriosis (can cause periureteral fibrosis)
- History TB (can cause multifocal strictures)
- Prior surgery with risk for ureteral injury
- Prior UPJ surgery (affects treatment decision)
Imaging considerations
- CT/US to assess degree of anatomic obstruction, crossing vessel (do not need to confirm preop), mass
- NM renal scan (MAG3): to assess split function and severity of obstruction (Lasix T 1/2)
- Antegrade/retrograde: obtain simultaneously to assess location and length of stricture, assists with planning surgical repair
- Whitaker test: position prone, perfuse saline at 10mL/min via PCN, drain bladder with catheter, monitor pressures in renal pelvis, nonobstructed = 12-15cm, obstructed > 22cm, useful for otherwise equivocal obstruction
General management recommendations:
- Indications for treatment: symptomatic obstruction, worsening renal function, stones, infection, persistent hypertension
- Nephrectomy: consider if < 15-20% split function
UPJ Obstruction Management
Pyeloplasty
- Goal: widely patent anastomosis with watertight closure without tension
- Nephrostomy tube: only recommended if infection, severe pain, or worsening renal function (pelvic distension improves operative dissection)
- Techniques: Anderson Hynes dismembered pyeloplasty most common, but can perform Y-V, spiral flap
- Ureterocalycostomy: indicated for small intrarenal pelvis, horseshoe kidney, or salvage procedure
- Drain placement: consider to prevent urinoma formation, but do not place on suture line (creates fistula)
Endopyelotomy
- Technique: perform full-thickness lateral incision (avoids hilar vessels) into peripelvic fat, incise with laser or wire balloon
- Leave stent (tapered if possible) for ~4-6 weeks
- Pyeloplasty failure: reasonable option, no difference in outcomes even if prior pyeloplasty
- Consider antegrade access if simultaneous stone treatment required
- Contraindications: long stricture (> 2cm), active infection, coagulopathy, crossing vessel
Postop management
- Tube plan: usually remove foley first, confirm no increased drain output after foley removal, leave stent for 4-6 weeks
- Follow-up: repeat renal scan 1mo after stent removal, then follow up at 6mo then annually for 2-3yrs (will catch most failures)
- Renal US may show persistent hydronephrosis, renal scan is better study to confirm resolution of obstruction and check for recurrence
- Success rates: > 90% for pyeloplasty, 79-88% for endopyelotomy
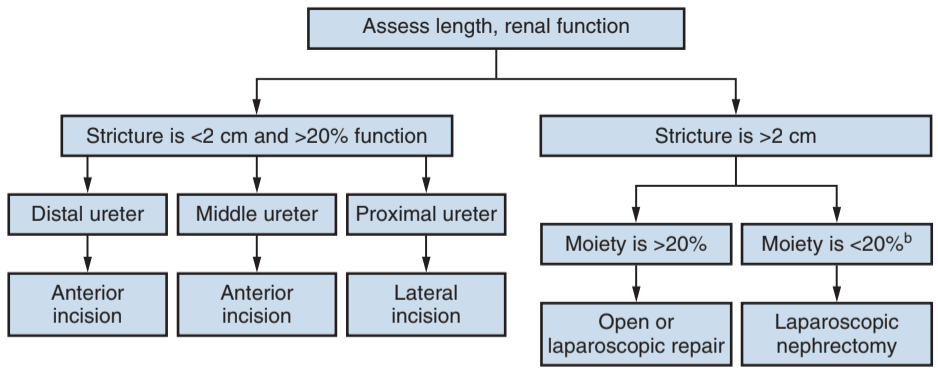
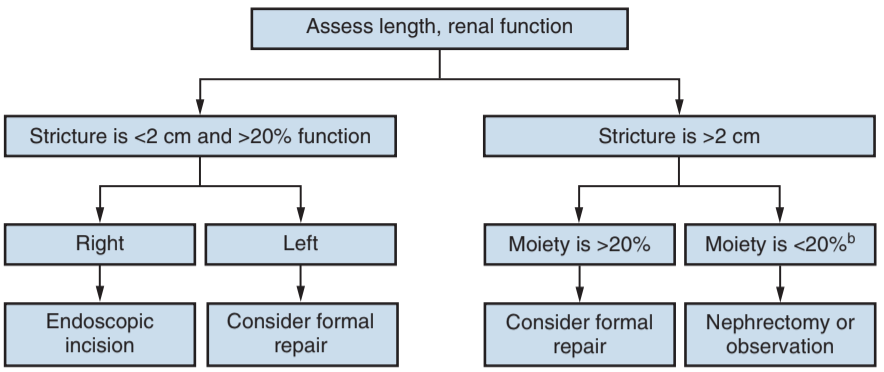
Algorithm for treatment of benign ureteral strictures, from Campbell's
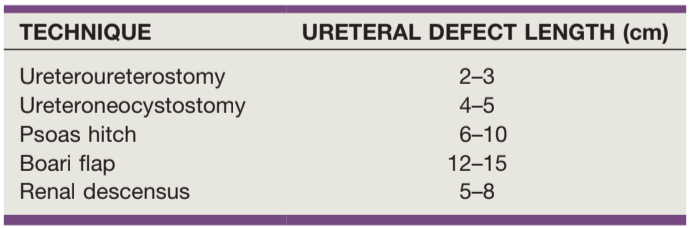
Stricture length treated with each repair, from Campbell's
(Benign) Ureteral Stricture Management
Endoscopic management
- Stent placement: successful in most (80+%) cases, metallic stents require less frequent exchanges, can be used as alternative to repair in properly selected patients
- Retrograde balloon dilation: option for short strictures (< 2cm) but may require multiple procedures, use 4cm 12-30Fr balloon, inflate for 10min at stricture site, leave stent for 2-4 weeks, success 50-85%
- Endoureterotomy: incise away from major vessels (proximal = lateral, distal = anterior), can use cold knife or laser, success 66-83%
- Follow-up: US or NM scan at 1mo after stent removal, then 3 and 6mo
Open repair
- Ureteroureterostomy (UU): upper/mid strictures, perform spatulated tension-free anastomosis with running stitch x2, leave foley and drain for 1-2 days, success rates 90%
- Transureteroureterostomy (TUU): contraindicated with hx stones, RPF, malignancy, prior XRT, chronic pyelo, correct reflux if present, tunnel donor ureter under sigmoid mesentery proximal to IMA and minimize mobilizing recipient ureter
- Ureteroneocystotomy: distal strictures, includes any reanastomosis of ureter to bladder, more difficult with small/contracted bladders, no benefit for antireflux repair
- Psoas hitch: provides 5cm extra length, may require ligation contralateral bladder pedicle, avoid suturing genitofemoral nerve
- Boari flap: provides 10-15cm extra length, useful when defect extends proximal to pelvic brim
- Renal mobilization: rotate inferiorly and medially on vascularpedicle, then hitch lower pole to retroperitoneal muscle
- Ileal ureter: anastomose isoperistaltic segment, less reflux if > 15cm used, contraindications are CKD, BOO, IBD, and XRT enteritis, can perform bilaterally with use of one long segment (reverse 7 technique), consider endoscopic surveillance for malignancy starting after 3yrs
- Buccal graft: rare, cover with omental flap
- Autotransplant: anastomose via gibson, can anastomose renal pelvis directly to bladder
- Stent: leave for 4-6 weeks in most situations
Specific causes of ureteral obstruction
Ureteroenteric anastomotic stricture
- Prevalence: 4-9%, more common on left side (greater tension)
- Workup: perform loopogram, antegrade nephrogram, or CTU to assess degree of obstruction and rule out malignancy, differentiate from expected obstruction due to refluxing anastomosis
- Nephrostomy tube: may be beneficial relieve obstruction and better assess degree of obstruction
- Management: consider endoscopic (laser vs balloon) if > 6-12mo initial surgery and stricture < 1-2cm, otherwise perform definitive surgical repair
- Success: 75% for open repair vs 15% for balloon dilation at 3yrs
Retroperitoneal fibrosis
- Develops near L4-L5 near aorta, causes extrinsic ureteral compression
- Presentation: can present with back/flank pain, weight loss, DVT and leg edema, HTN, hematuria, pain relieved by aspirin
- Imaging: CT, IVP, RGPG will show medial deviation of ureters, RPF best characterized with MRI
- Medical management: refer to rheumatology, mainly use steroids but may require other immunosuppresants, 80% show clinical improvement, 60mg daily tapering to 5mg daily, 50% relapse rate
- Ureterolysis: start distally and work proximally, use split and roll technique, consider wrapping with omentum or intraperitonealizing ureters, 90+% success for relieving obstruction
Malignant obstruction
- Stent failure: occurs in 24-44% stent placement (compared to 10% for benign disease)
- Metal coil stents: more resistant to compressive forces, do not require as frequent exchanges, MRI compatible
- Surveillance: perform pyelogram (antegrade/retrograde) to assess continued need if obstruction adequately treated
Infundibular stenosis
- Causes: prior PCNL (occurs ~2%), chronic inflammation, congenital
- Fraley syndrome: intrarenal crossing vessel obstructs upper pole infundibulum
- Imaging: CT/US, dilated calyx with non-dilated pelvis
- Repair indications: worsening renal function, pain, infection, stones
- Management: balloon dilation, endoscopic incision (avoid anterior/posterior incisions), surgical repair, partial/total nephrectomy, chronic stent/PCN
References
- AUA Core Curriculum
- Nakada, S. and S. Best. "Management of Upper Urinary Tract Obstruction." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.