Genitourinary Trauma
Renal Trauma
| IF... | THEN... | |
|---|---|---|
| Diagnosis | Blunt trauma + GH | Obtain CTU |
| Blunt trauma + MH + SBP < 90 | ||
| Blunt trauma concerning for renal injury but no hematuria | ||
| Penetrating trauma near kidney with(out) hematuria | ||
| Exam (rib fx, flank bruising) concerning for renal injury | ||
| Unstable patient taken to OR without imaging | Obtain on table IVP 2mL/kg contrast bolus XR 10-15min later |
|
| MH, no hypotension, no concerning injury | Can observe without imaging | |
| Management | Grade I-III injury | Manage conservatively |
| Grade IV-V injury | Repeat CT within 48hrs | |
| Fever | ||
| Worsening flank pain | ||
| Worsening anemia | ||
| Abdominal distension | ||
Expanding urinoma with:
|
Provide GU drainage Stent preferred Can consider PCN or drain |
|
| Urinary extravasation without above signs | Can manage conservatively | |
| Hemodynamically unstable not responding to resuscitation | Absolute indication for embolization/exploration | |
| Hemodynamically unstable + perirenal hematoma > 4cm or Grade 3-5 injury with contrast extravasation | ||
| Expanding/pulsatile renal hematoma | ||
| Suspected vascular pedicle avulsion | ||
| UPJ avulsion | ||
| Urine extravasation with significant parenchymal devascularization | Relative indication for embolization/exploration | |
| Renal + colon/pancreas injuries | ||
| Arterial thrombosis | ||
| Urine extravasation from parenchymal injury |
CT findings concerning for major renal injury (9x more likely to require intervention)
- Medial hematoma: suggests vascular injury
- Medial urinary extravasation: suggests renal pelvis or UPJ avulsion
- Global lack of parenchymal enhancement: suggests renal artery occlusion
- Combination of 2+: large hematoma > 3.5cm, medial renal laceration, vascular contrast extravasation
Post-renal injury hypertension mechanisms (renin production stimulated by partial ischemia)
- Goldblatt kidney: renal artery injury leading to stenosis/occlusion
- Page kidney: compression of renal parenchyma with blood/urine
- Arteriovenous fistula: decreased renal perfusion due to diversion
Renal injury tips
- Prevalence: up to 34% have renal injury without hematuria or hypotension
- Venous injury: CT is not sensitive, have high suspicion in presence of medial hematoma
- Intraoperative IVP: confirms presence of contralateral kidney prior to performing trauma nephrectomy
- Embolization failure: seen in 13-88%, can repeat embolization
- Pseudoaneurysm: may develop in up to 2.5% renal trauma
- Fluid collections: urinoma (0-20 HU, delayed contrast pooling), hematoma (> 30 HU), abscess (rim enhancement + > 20 HU with contrast)
- During exploration, isolation/control of renal vessels prior to renal exposure no longer necessary
- Surgery tips: can attempt renal repair with debridement, suture ligation, closing collecting system and parenchymal defects, flaps, and drain placement
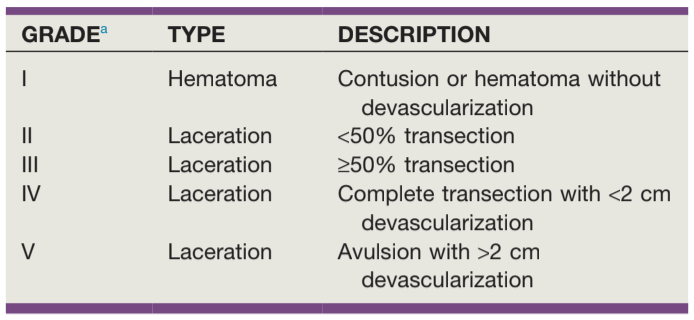
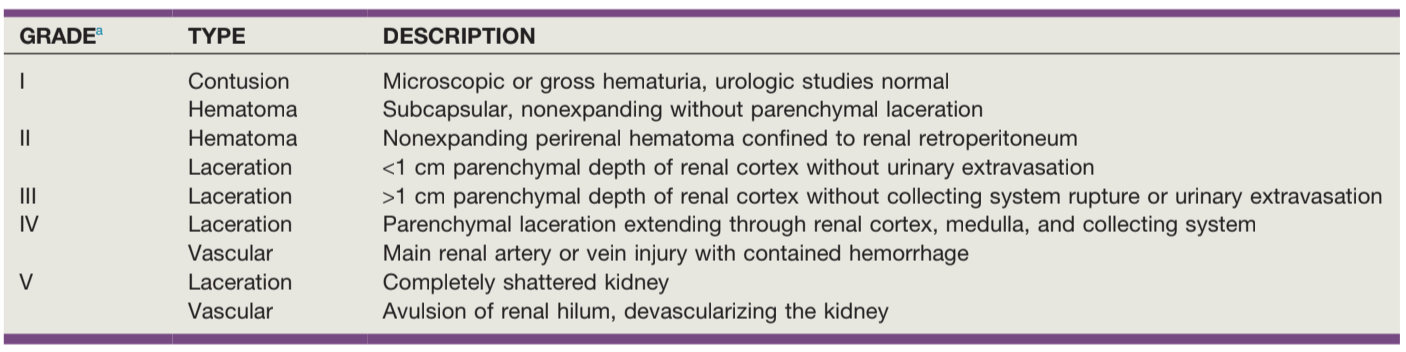
AAST ureteral injury severity, from AAST + Campbell's
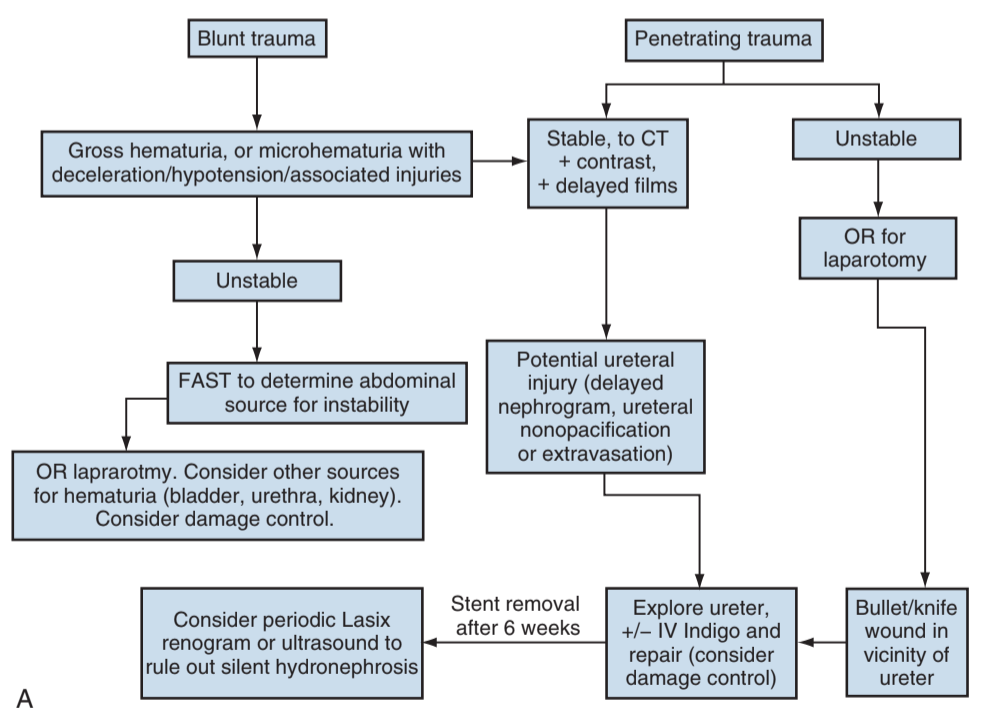
Algorithm for ureteral injury from external trauma, from Campbell's
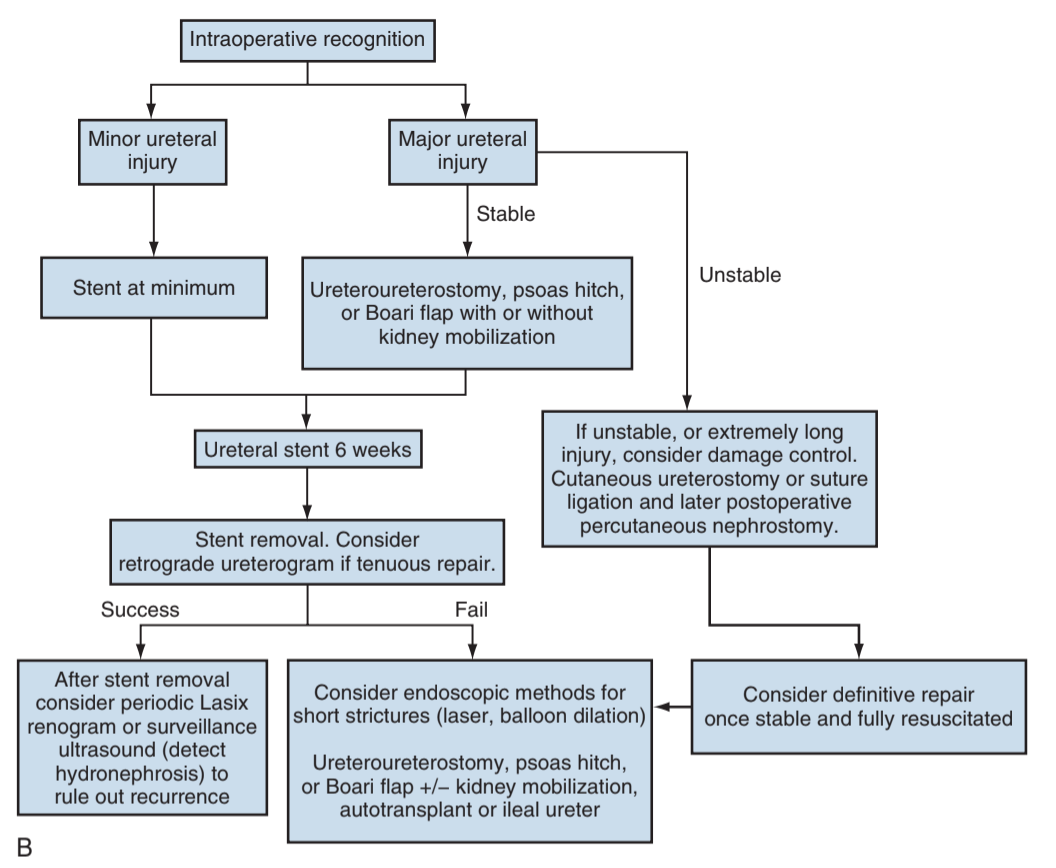
Algorithm for iatrogenic ureteral injury discovered intraoperatively, from Campbell's
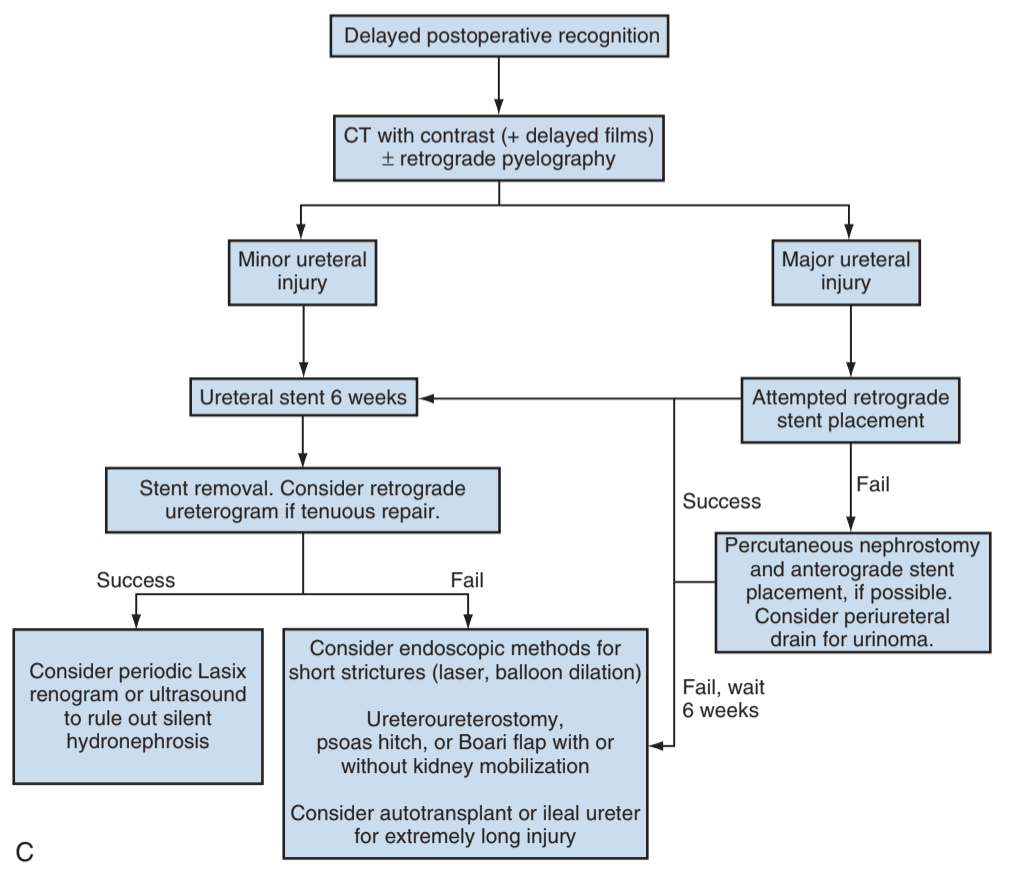
Algorithm for iatrogenic ureteral injury discovered postoperatively, from Campbell's
Ureteral Trauma
| IF... | THEN... | |
|---|---|---|
| Diagnosis | Ureteral injury suspected (see renal criteria) | CT urography |
| Assessing for intraoperative injury | Inspect ureter Inject dye IV or via renal pelvis Contrast evaluation |
|
| Management | Stable + contusion or crush injury | Place stent Debride if large injury |
| Stable + intraop laceration | Place stent Repair laceration |
|
| Unstable + intraop injury | Ligate ureter with nonabsorbable stitch Place PCN or cutaneous ureterostomy +/- stent Delayed repair |
|
Delayed identification:
|
Retrograde pyelogram + stent placement If fails, place PCN Delayed repair |
|
| Ureterovaginal fistula | Stent (64-76% success) Delayed repair (100% success) |
Prophylactic stenting
- Does not decrease risk for injury, but improves chances of identifying injury
- Anuria risk with bilateral stents: 1-5% (place over a wire to minimize trauma)
- Ureteral injury during placement: 1%
- Inability to place stent: 13% unilateral, 2% bilateral
Ureteral repair principles
- Avoid ureteral devascularization
- Minimize debridement but assess for vascularity
- Perform spatulated, tension-free, stented, watertight anastomosis
- Close peritoneum if possible
- Place drain to evaluate for leak
- Do not tunnel ureteroneocystotomies
- Consider omental flap for severe injuries
Ureteral injury tips
- Remove catheter, then drain, to prevent urinoma formation
- Either repair immediately or delay repair for 6-8 weeks due to inflammation
- Distal injuries may require reimplantation
- Endoscopic iatrogenic injuries may heal with stenting alone
- Absence of hematuria and presence of bilateral jets is a poor predictor of injury, but can consider visualizing efflux of dye for confirmation
Bladder Trauma
| IF... | THEN... | |
|---|---|---|
| Diagnosis | Pelvic fracture + gross hematuria | Retrograde cystography |
| Penetrating injury to butt, pelvis, lower abdomen + any hematuria | ||
| Management | Intraperitoneal injury | Immediate surgical repair |
| Pelvic fracture + bone fragments in bladder | ||
| Simultaneous rectal/vaginal injury | ||
| Bladder neck injury | ||
| Laparotomy for non-bladder reasons | ||
| Inadequate drainage or clots | ||
| Penetrating trauma | ||
| Extraperitoneal injury | Catheter x2-3 weeks (avoid exploration if possible to prevent severe bleeding) | |
| Prolonged catheterization required | Consider suprapubic tube placement | |
| Neurologic injuries | ||
| Orthopedic injury + immobility | ||
| Complex bladder closure | ||
| Iatrogenic endoscopic injury | Extraperitoneal perforation | Catheter drainage |
Small intraperitoneal perforation without:
|
Catheter drainage + antibiotics | |
| Large intraperitoneal perforation | Surgical repair | |
| Small intraperitoneal perforation with above criteria | ||
| Extraperitoneal perforation failing to heal |
Cystography tips
- Technique: fill w/ 300-350mL or to discomfort, do not fill passively with IV contrast
- XR Cystography: image at pre-fill, max fill, and after emptying, obtain 2-view images
- CT cystography: drainage films not required, dilute contrast 6:1 otherwise can create scatter artifact
- Findings: extraperitoneal injury with flame-shaped collection in pelvis, intraperitoneal injury with contrast outlining bowel loops
Bladder injury tips
- Hematuria: not always present (77-100%)
- Bladder rupture: > 90% will have gross hematuria, 0.6-5% will have microscopic hematuria only, seen with 29% patients with pelvic fracture + gross hematuria
- Pelvic fracture: seen in 83-95% bladder injuries, but bladder injury present in 5-10% pelvic fractures, suspect if circle displacement > 1cm, pubic symphysis diastasis > 1cm, or pubic rami fracture
- Unrecognized bladder injury signs: acidosis, azotemia, fever, sepsis, low UOP, peritonitis, ileus, ascites, respiratory distress, incontinence, fistula, stricture
Surgery tips
- Principles: place catheter, inspect bladder neck and ureteral orifices for injury, minimize debridement, close with absorbable suture, perform leak-test
- Simultaneous vaginal/rectal injury: place omental flap or other interposition to prevent fistula
- Catheter duration: obtain cystogram 10-21 days after surgery to assess for leak
Urethral Trauma
| IF... | THEN... | |
|---|---|---|
| Diagnosis | Blood at meatus | Immediate retrograde urethrogram Do not place catheter before RUG |
| Pelvic fracture | ||
| Bladder rupture | ||
| Genital/perineal hematoma | ||
| Penile fracture | ||
| High-riding prostate | ||
| Penetrating penile injury | ||
| Distended bladder | ||
| Management | Partial urethral disruption | Attempt catheter placement once Then place SPT |
| Penetrating anterior injury | Consider immediate repair if able Delay if unstable, extensive tissue loss, or lack of experience |
|
| Pelvic fracture + urethral injury | Place SPT (preferred options) Primary repair if rectal/bladder neck injury present |
|
| Straddle injury | Place urethral or SP catheter | |
| Penile fracture with urethral injury | Immediate repair |
Retrograde urethrogram instructions
- Bottom leg flexed, top leg straight, oblique angle
- Small catheter placed in meatus (12Fr)
- Gentle traction, inject 20mL undiluted contrast
- If catheter already placed, use 3Fr catheter next to indwelling catheter
Urethral injury tips
- Pelvic orthopedic repair: NOT a contraindication to SPT placement
- Delayed repair: perform 2-3mo after injury (stable scar tissue), evaluate with simultaneous urethrogram and VCUG
- Primary realignment: high risk for stenosis, place and maintain SPT, can remove 1-2 weeks later
- Endoscopic stricture management: rarely successful
- Long term management: monitor for ED (50-82%), strictures (5-15%), incontinence (< 4%) for at least 1yr after injury
Penile Trauma
Fractures
- Diagnosis: suspect when bruising/edema, reported "pop" with immediate loss of erection, obtain US if diagnosis equivocal
- Taqaandan: self-inflicted fracture, penis forcibly bent during masturbation as a method to achieve rapid detumescence
- Management: can take to OR on clinical evidence alone, imaging not required, US preferred for equivocal findings
- Incision: make ventral incision (most common fracture location), localized incision over hematoma, or subcoronal incision
- Urethral injury: can perform intraoperative cystoscopy or preoperative urethrography (time-consuming)
- Close tunical defects with 2-0 or 3-0 absorbable sutures, smaller for urethral injury
- Mimics: rupture of dorsal penile artery, dorsal penile vein, or suspensory ligament
- Surgical delay: up to 7 days does not adversely affect repair results
- Preventing postop erections: consider benzodiazepines, amyl nitrate, or ketoconazole
Penetrating trauma
- Management: exploration, irrigation, excision, surgical closure, antibiotics
- Urethral injuries: can be identified with urethrography or pericatheter dye injection, can repair primarily
- Animal bites: irrigation/debridement, antibiotics (augmentin, cefoxitin, clindamycin + quinolone), do not close human bite wounds primarily
Amputation
- Psychosis: present in 65-87% patients, always consult psychiatry
- Ischemia time: successful if within 16hr for cold or 6hr for warm
- Double bag: wrap in saline-soaked gauze, place in bag, place in second bag with ice
- Microscopic repair: not required to anastomose and regain erectile function, but has less risk for strictures, skin loss, and sensory loss (20% vs 90-100%)
- Skin necrosis: high risk due to loss of blood supply
- Technique: SPT placement, close tunica with absorbable 2-0, close urethra with absorbable 4-0, dorsal artery with 11-0 nylon, dorsal vein with 9-0 nylon, dorsal nerve with 10-0 nylon, skin coverage
Zipper injuries
- First tricks: perform penile block, lubricate with mineral oil, attempt to unzip
- Second tricks: cut cloth between each individual tooth to release support and have zipper fall apart
- Third tricks: consider cutting median bar of zipper with a bone cutter or wire cutter, or screwdriver to pry apart top and bottom
Strangulation injuries
- Examine any idiopathic penile swelling for hidden hair or string
- Attempt reduction of distal edema with penile wrap
- String reduction technique: useful if able to thread string under constricting device, can also puncture glans to drain edematous blood/fluid
- Can incise plastics with scalpel or cast saw
- Metal items may require industrial cutting devices, including from fire or EMS services, perform in OR under anesthesia
- Consider suprapubic tube if patient unable to void and removal delayed
Scrotal/Testis Trauma
Rupture
- Scrotal US: assess for hematoma, incongruity of tunica albuginea, loss of contour, heterogenous parenchyma
- Indications for OR exploration: penetrating injury, scrotal US unable to rule out rupture, hematoma actively enlarging or > 5cm
- Technique: debride extruded tissue, close with 4-0 absorbable suture, consider drain placement, perform orchiectomy if non-viable appearance
- Success: 80-90% salvage rate if explored within 3 days of injury, 32-65% salvage rate for penetrating trauma
- Dislocation: due to high-impact trauma to scrotum, consider imaging with US/CT to find testis if empty hemiscrotum present on exam, explore via inguinal incision and perform orchiopexy
Scrotal skin loss
- Debride non-viable tissue and attempt primary closure
- Thigh pockets: consider on loss of > 50-60% scrotal skin
- Skin grafting: split thickness preferred
- Deep electrical burns: manage conservatively, often leads to autopenectomy or death due to severity of total injuries
Scrotal hematoma/hematocele
- Prevalence: 80% hematoceles are caused by testis rupture and should be explored
- Hematocele: small collections can be observed, otherwise explore if large or persistent bleeding to prevent infection, testicular compression, prolonged pain
- Cutaneous hematoma management: ice, elevation, scrotal support
- Intratesticular hematoma management: difficult to distinguish from testis rupture, therefore requires scrotal exploration, can re-image in 4-6 weeks to assess for resolution (vs concern for testis tumor)
References
- Brandes, S. and J. Eswara. "Upper Urinary Tract Trauma." Campbell-Walsh Urology 12 (2020).
- Morey, A. and J. Simhan. "Genital and Lower Urinary Tract Trauma." Campbell-Walsh Urology 12 (2020).
- Morey, Allen F., et al. "Urotrauma Guideline 2020: AUA Guideline." The Journal of Urology 205.1 (2021): 30-35.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.