Male Stress Urinary Incontinence
Post-Prostatectomy Expectations
Incontinence
- Continence: 90% by 6mo, 94% by 12mo, 95% by 24mo
- Kegels: start 3-4 weeks prior to surgery for best results
- XRT: worsens incontinence rates
- Salvage prostatectomy: 20-70% incontinence rate
Climacturia
- Prevalence: ~30% (range 20-93%), 50% report as bothersome, 33% avoid sexual situations
- SUI: 70% SUI also report climacturia...and 70% climacturia report SUI
- Robotic surgery decreases time to no climacturia
- Risk factors: prior TURP, shorter urethral length
- Management: pre-sex urination, condoms, PFPT
Workup + Evaluation
History
- Symptoms: duration, frequency, severity (PPD, pad type), precipitating factors
- Self-reported hx SUI: 95% PPV, 100% NPV
- Prior prostatectomy: 5% will have persistent SUI 2yrs after surgery
- Prior TURP: SUI 0-8%, up to 70% have reported some urge incontinence
- Medications: a-blockers, diuretics, anticholinergics
- Associated symptoms: assess sexual, erectile, and bowel function
- UUI: 29-48% with SUI also report OAB symptoms
Further Workup
- Exam: assess cognitive function and manual dexterity, inguinal hernias, prior surgical scars, neuro exam
- DRE: check prostate (if present), rectal tone, and pelvic floor dysfunction
- Post-void residual: check to ensure patient does not have overflow incontinence
- Bladder diary: 3-days is adequate, can use for UUI or unclear symptoms
- Pad weight: assess severity, < 200g mild, 200-400g moderate, > 400g severe
- UA/UCx: treat UTI prior to surgery
- Cystoscopy: required preop or intraop, assess for stricture, bladder neck contracture
- Urodynamics: use only if it would affect treatment options, 35% patients will not demonstrate SUI while UDS catheter is in place (bladder neck contracture may be present)
Artificial Urinary Sphincter
Preoperative planning
- Consider anti-incontinence surgery at 12mo, but can offer as early as 6mo
- Assess: BMI, prior surgery/XRT, SUI severity
- poor manual dexterity or cognitive function, high surgical risk, bladder neck contracture, poor compliance, VUR at low pressures, bladder cancer (relative)
- Bladder neck contracture: repair prior to any incontinence treatment, and confirm success with cystoscopy
Success
- PPD: median 4 PPD preop, down to median 0.6 PPD postop
- Success: full continence (20%), few drops of leakage (55%), less than a teaspoon leakage (22%)
- Satisfaction: 92% would undergo again, 96% would recommend to a friend
- Prior XRT: AUS has better results than sling (continence 56% vs 89%) but increased revision rate overall (HR=1.56)
Complications
- Device failure: normal life expectancy 7-10yrs, 24% at 5yrs, 50% at 10yrs
- Retention: rare, often due to stricture or bladder neck contracture
- Infection: 1-5%, explant immediately, can perform immediate or delayed (3-6mo) reimplant
- Erosion: 1-10%, risks include prior XRT (use lower pressure reservoir), DM, CAD, and prior revisions, presents with hematuria, dysuria, or retention, explant and place catheter with possible intraop urethral repair, delay reimplant by 3-6mo
- Urethral atrophy: slowly worsening incontinence, manage with downsizing, repositioning, transcorporal placement or tandem placement, do not increase reservoir pressure
- Persistence incontinence: accidental deactivation, fluid loss, or improper cuff sizing
- Recurrent incontinence: fluid loss, urethral atrophy, or cuff erosion
- Fluid loss: assess for balloon leak with CT or US imaging
- Cystoscopy: consider to assess erosion or atrophy, cycle cuff
- Revision: 25%, consider cuff resizing, adjusting position, tandem cuff, or transcorporal approach
- Urinary diversion: multiple AUS failures, intractable BNC, detrusor instability
Non-AUS Therapies
Conservative therapies
- Kegels: can start before prostatectomy, decrease time to regaining continence but do not improve overall chances of regaining continence
- Pelvic Floor PT: consider as adjunct if mild SUI
- Catheters: useful for high volume leakage and skin breakdown but should be last resort, SPT will not work if patient has sphincteric incompetence
- Condom catheter: may provide improved quality of life but require proper sizing
- Clamps: release every 2 hours to prevent erosion and do not wear overnight (urethral erosion), do not use if patient has memory deficits, poor manual dexterity, impaired sensation, or OAB symptoms
- Pads: variety of options for patient preferences, but even 1 PPD may be bothersome
Sling
- Indications: mild/moderate incontinence (24hr pad weight < 150-400g), not recommended for prior XRT or urethral erosion
- Patient preference: all else being equal, most men (2%) prefer sling placement due to AUS complication risk
- Success: 50-60% dry, 25% improved but not dry, lower rates if prior XRT or severe SUI
- Failure: if sling fails, AUS has lower failure rate than repeat sling (6% vs 55%)
- Complications: urinary retention (0-44%, resolves within 1 week), pelvic/perineal pain (12-17%, most resolve within 12 weeks), erosion/infection (1-2%)
Bulking agents
- Agents: bovine collagen, macroplastique
- May require repeat injections
- Efficacy: full continence (17%), improvement (50%), increased leakage (1.5%)
- Complications: retention, frequency, dysuria, UTI
Balloon
- Option for mild incontinence
- Efficacy: 60-81% report 0-1 PPD
- Explant rates: 4-20%
References
- AUA Core Curriculum
- Al-Mousa, R. and H. Hashim. "Evaluation and Management of Men with Urinary Incontinence." Campbell-Walsh Urology 12 (2020).
- Boone, T., J. Stewart, and L. Martinez. "Additional Therapies for Storage and Emptying Failure." Campbell-Walsh Urology 12 (2020).
- Cameron, A. "Complications Related to the Use of Mesh and Their Repair." Campbell-Walsh Urology 12 (2020).
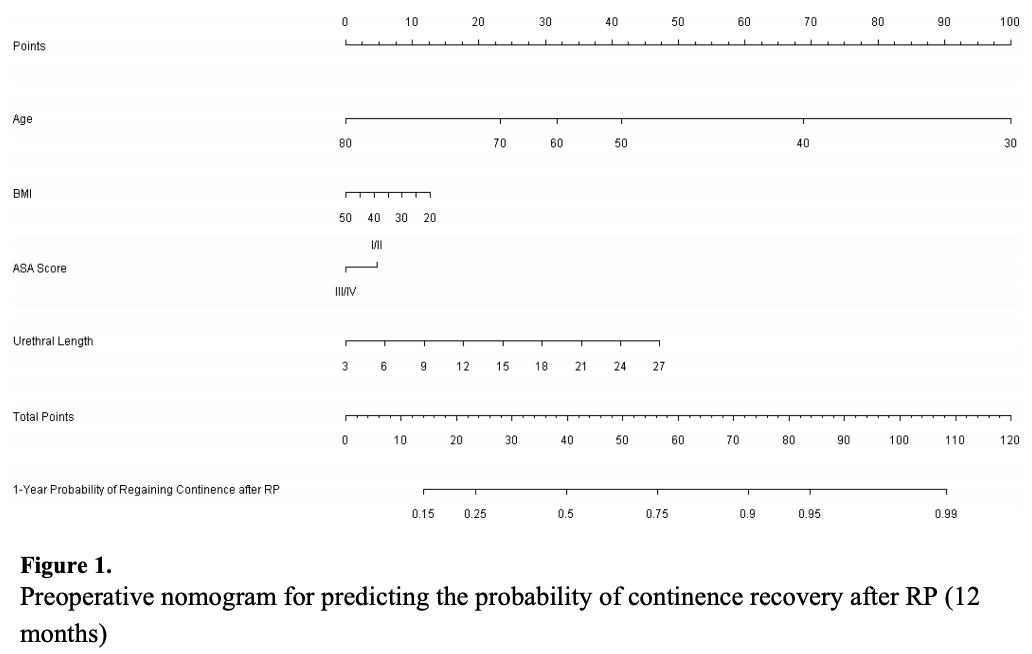
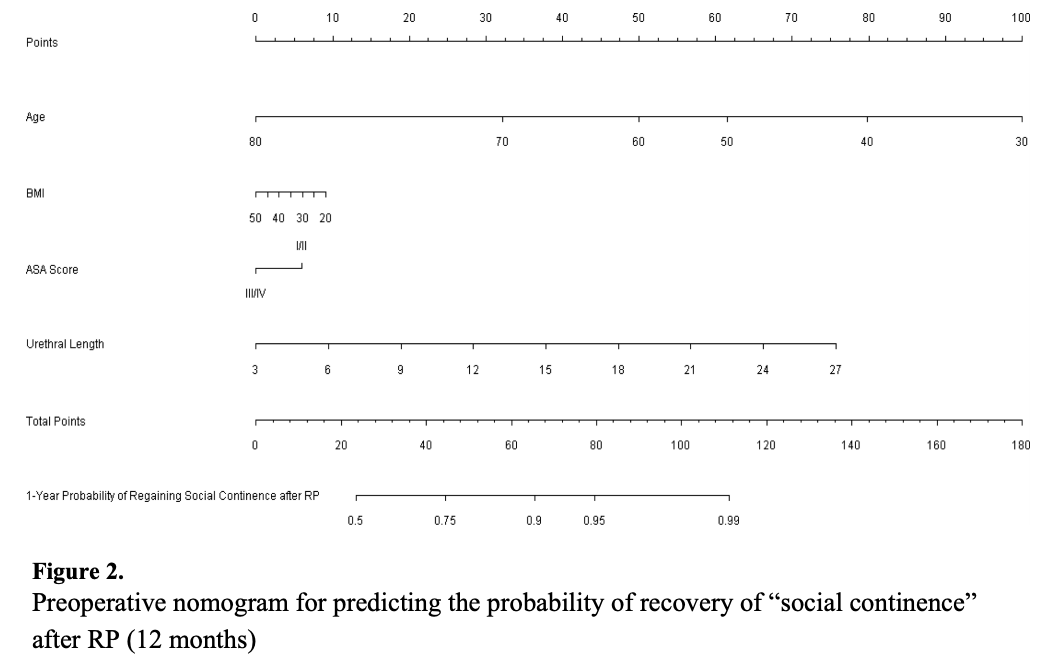
- Matsushita, Kazuhito, et al. "Preoperative predictive model of recovery of urinary continence after radical prostatectomy." BJU international 116.4 (2015): 577-583.
- Sandhu, Jaspreet S., et al. "Incontinence after prostate treatment: AUA/SUFU Guideline." The Journal of urology 202.2 (2019): 369-378.
- Wessells, H. and A. Vanni. "Surgical Procedures for Sphincteric Incontinence in the Male." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.