Diverticula
Bladder Diverticula
Types
- Congenital diverticula seen by ages 10 or younger, associated with reflux, outlet obstruction, voiding dysfunction, have isolated diverticulum with smooth-walled bladder
- Acquired diverticula secondary to outlet obstruction or voiding dysfunction, seen in setting of bladder trabeculation
- Hutch diverticulum: superolateral to ureteral orifice without trigonal involvement in setting of neurogenic bladder and reflux
Diagnosis
- May present with variety of voiding symptoms, UTI, stones
- Can be directly visualized endoscopically
- Consider VCUG to assess outlet obstruction, reflux, and filling/emptying of diverticulum
- Upper tract imaging warranted to assess for upper tract obstruction, seen in 7% (30% in pediatrics)
- Urodynamics may be useful, but can be confounded by diverticular filling/emptying during the study
- Malignancy present in 1-10%
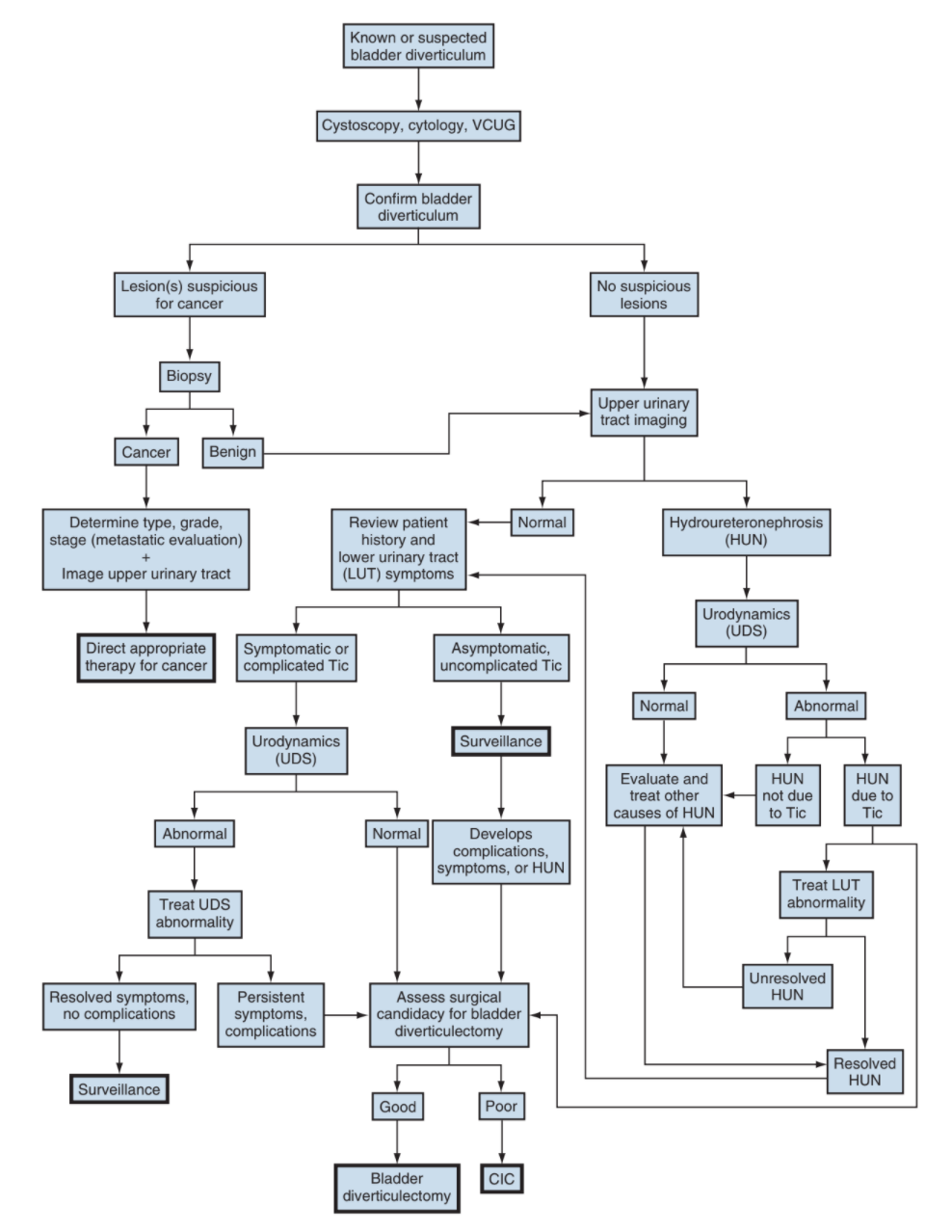
Management
- Treating outlet obstruction may avoid need for treatment of diverticulum
- Indications for diverticulectomy: symptoms related directly to diverticulum, recurrent UTIs, stones, cancer, upper tract obstruction
- Biopsy of malignancy has increased risk for perforation due to lack of detrusor muscle, can consider diverticulectomy versus radical cystectomy
- Transurethral incision/resection of diverticular neck can open up diverticulum and improve emptying, can fulgurate diverticular lining to decrease size
- Surgical excision can be performed via any approach
Female Urethral Diverticula
- Prevalence 1-6%
- Periurethral cystic structure connected to urethra by an ostium
- Unclear cause, likely due to blocked periurethral ducts that rupture and fistulize with urethral lumen, but periurethral cysts are uncommon
- Stones found in 4-10% cases
Evaluation
- Only 5% present with dysuria + dyspareunia (12-24%) + post-void dribbling (5-32%)
- Other symptoms include LUTS, UTI, urethral/vaginal mass, hematuria, urinary retention
- Assess history pelvic surgery, bulking agents, sexual symptoms
- Perform vaginal exam,, assess anterior vaginal wall, no benefit to "urethral milking"
- Cystoscopy is optional, ostium may be identified in only 15-89%, exam may be painful
- MR imaging is gold standard, needs diverticulum protocol for best imaging results
- Alternate imaging modalities: VCUG, transvaginal US
- LNSC3: location, number, size, anatomic configuration, communication with lumen, and continence status
Differential
- Skene gland cyst: drains adjacent to urethra with meatus distortion, manage with aspiration, marsupialization, or excision
- Gartner duct cyst: mesonephric remnant in anterior vaginal wall, may drain an ectopic ureter, manage with aspiration/sclerotherapy or excision
- Urethral prolapse: circumferential meatal herniation, beefy red appearance, may cause spotting, seen in prepubertal girls and postmenopausal women, manage with topical estrogen/NSAIDs, sitz baths, and excision
- Urethral caruncle: reddish exophytic mass at meatus, can cause spotting, manage with topical estrogen/NSAIDs, sitz baths, and excision
- Bulking agents: may present as periurethral bulge, can be confused on imaging, patient history is key
- Vaginal leiomyoma: freely mobile mass on anterior vaginal wall, estrogen-dependent, can enucleate to rule out malignancy
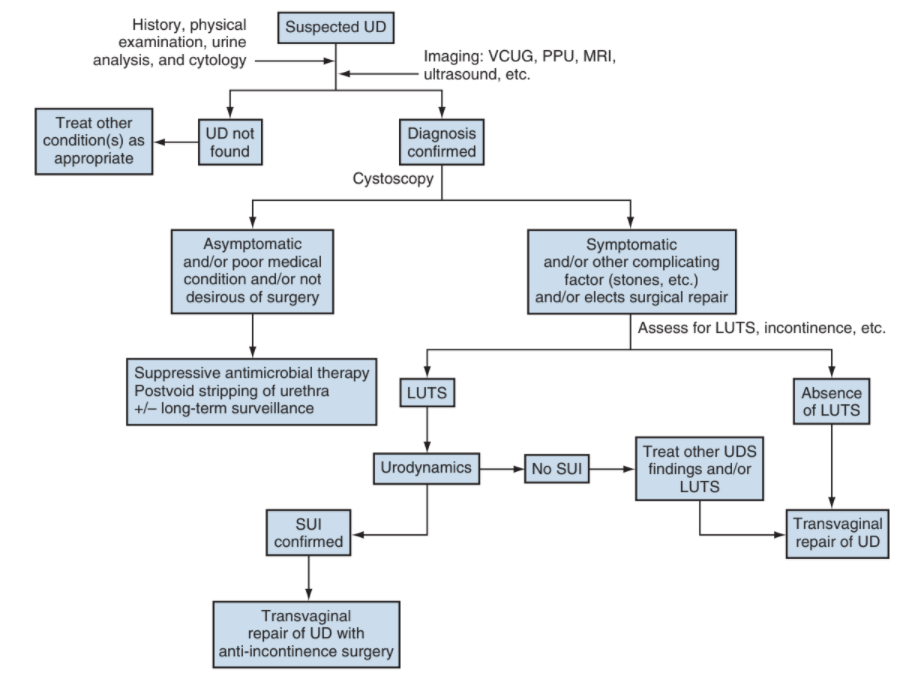
Management
- If patient opts for observation, discussion low but potential risk for developing cancer
- If SUI, can perform pubovaginal sling at time of diverticulectomy
- Can perform transvaginal excision or marsupialization
- Maintain catheter drainage 2-3 weeks, consider VCUG prior to catheter removal
- Excision complications: incontinence (2-16%), fistula (1-8%), stricture (0-5%), recurrence (10-22%), UTI (0-31%)
Urethral diverticular cancer
- Less than 100 cases reported
- Adenocarcinoma most common (primary urethral cancer most often squamous cell)
- Management: diverticulectomy, radical cystourethrectomy, XRT, chemotherapy
References
- AUA Core Curriculum
- Cox, L. and E. Rovner. "BLadder and Female Urethral Diverticula." Campbell-Walsh Urology 12 (2020).