Kidney Disease and Transplantation
Acute and chronic kidney disease
Acute kidney injury (AKI)
- History: fluid intake, voiding history, bowel history, hematuria, flank pain, systemic symptoms, recent medications
- Exam: blood pressure, mental status, edema/turgor, flank pain, abdominal mass, rash
- Adjuncts: CBC, electrolytes (include Ca/Phos), albumin, renal US, UA (and UCx), consider urine electrolytes, consider biopsy
- General management: supportive fluids, balance electrolytes, consider maximal drainage with catheter, stop nephrotoxic medications
- Hyperkalemia management: furosemide (1-2mg/kg IV), sodium bicarbonate (1mEq/kg), kayexelate (0.5-1g/kg PO or 1.5-2g/kg PR), check EKG, can also consider calcium gluconate (100mg/kg IV max 2g)
Chronic kidney disease (CKD)
- History: voiding habits, bowel habits, UTI, VUR, spina bifida, SLE, vasculitis
- Family history: CKD, cystic disease, dialysis, transplant
- Exam: flank/abdominal mass, suprapubic fullness, lumbosacral abnormalities, genital abnormalities
- Adjuncts: electrolytes (serum/urine), assess for hematuria/proteinuria, albumin, PTH, CBC, renal US, consider biopsy
- Hypertension management: salt restriction (< 2g/d), enalapril (0.1-0.5mg/kg/d PO, dosed BID), amlodipine (0.1-0.5mg/kg/d PO, dosed QD or BID), furosemide (0.5-1mg/kg PO BID)
- Osteodystrophy: restrict phosphorus (< 15mg/g protein daily), sevelamer (400-1600mg/meal), calcitriol (0.25-1.0mcg/kg/d)
- Acidosis: sodium citrate for infants (1-3mEq/kg/d dosed TID), otherwise sodium bicarbonate (1-2mEq/kg/d dosed TID)
Kidney Transplants
Preparation
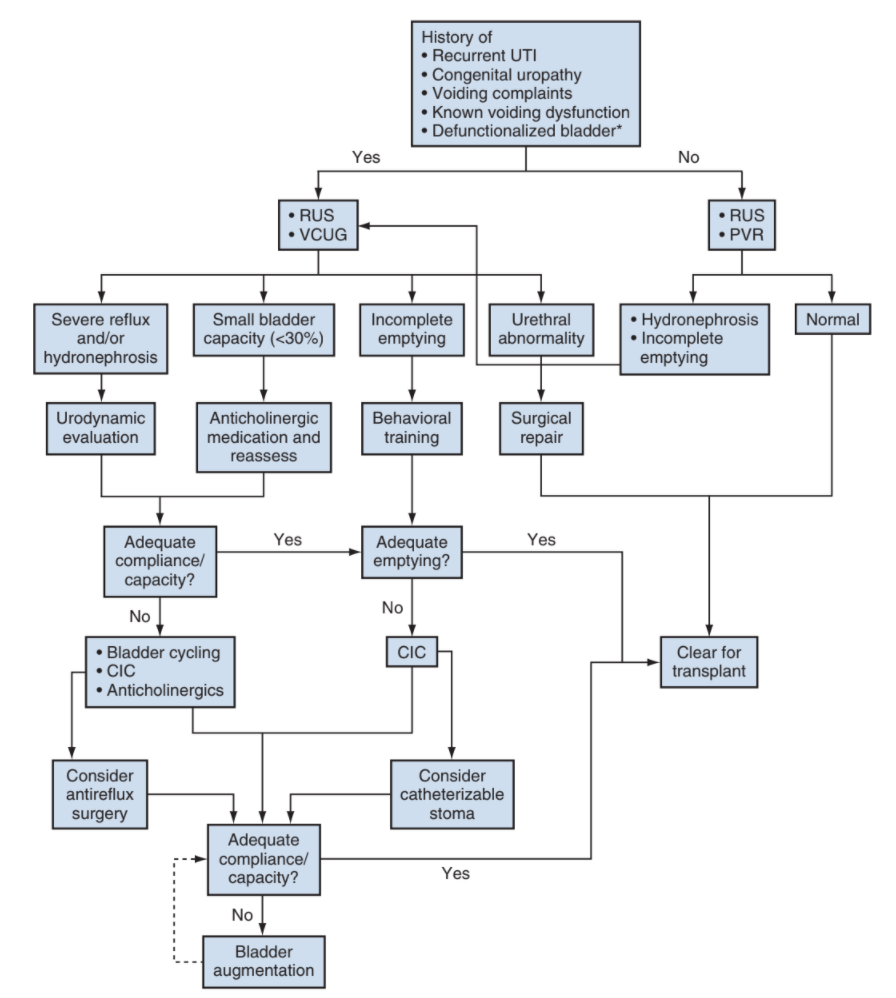
- Urodynamics: perform if known NGB, hx PUV, hx ureterocele, severe voiding dysfunction, high grade hydronephrosis, recurrent UTIs
- Most common bladder abnormalities in ESRD: low capacity, hypercontractility, poor compliance
- Bladder augmentation: may be beneficial in contracted bladders (capacity < 75% expected for age) and does not increase transplant complication risk, but must factor in location of pedicle and catheterizable channel so that they do not interfere with transplant
Procedural tips
- Anastomoses: renal vein to vena cava end to side, renal artery to common iliac end to side, ureter to bladder via extravesical approach (or donor to native ureter end to side)
- Indications for pretransplant nephrectomy: poorly controlled HTN, severe nephrotic syndrome, severe polyuria, recurrent upper tract infections, large stone burden, high malignancy risk, large kidneys (make room for transplant), severe reflux
- Stent is not required
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Peters, C. and A. Lorenzo. "Urologic Considerations in Pediatric Renal Transplantation." Campbell-Walsh Urology 12 (2020).