Pediatric Stone Disease
Considerations
- 50% will have a recurrence within 3-5 years of first episode
- Increased risk for CKD, decreased BMD, and heart disease
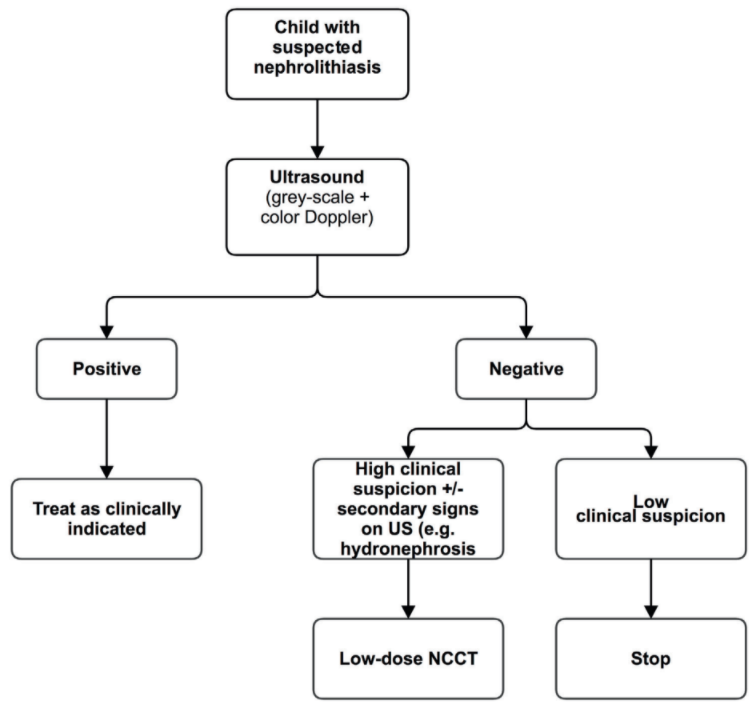
- Obtain CT imaging only if renal US is nondiagnostic and clinical suspicion is high
- US stone criteria: hyperechoic focus in kidney + twinkle artifact (multicolor signal on Doppler), up to 25% false positive rate (higher than adults)
- Neonatal nephrocalcinosis: seen in 7-41% preterm infants in NICU, most resolve spontaneously, only 15% will require further interventions
Urine stone workup findings
- 24hr urine indications: low utility in obtaining in first-time stone formers, recommend empiric diet counseling and only performing workups for patients with recurrent stone formation (Carnes 2021)
- Hypercalciuria: 4 mg/kg/day if > 2yo, Ca/Cr ratio > 0.21mg/mg
- Hyperoxaluria: primary may require liver/kidney transplant, secondary caused by increased gut absorption, Lumasiran (Oxlumo) can be started as early as 3mo for patients with primary hyperoxaluria
- Hypocitraturia: Cit/Cr ratio < 128mg/g in boys and < 300mg/g in girls
- Cystinuria: normal excretion < 60 mg/d/1.73m2 BSA
- Hyperuricosuria: leads to epitaxy (uric acid acts as nidus)
Prevention
- Fluids: up to 1.5-2L/m2 for cystinuria
- Sodium: limit to 2-3mEq/kg/d or 2.4g/d in teenagers/adults
- Calcium: maintain normal levels, low Ca may worsen stone risks
- Protein: do not exceed normal requirements
- Oxalate: majority (80%) does not come from diet, but can limit if proven hyperoxaluria
- Protective factors: citrate, potassium, magnesium
Medications
- Alpha blockers: can be given for acute stone episode if < 10mm, overall utility unknown
- Thiazides: hypercalciuria resistant to low sodium diet, 1-2mg/kg/d
- K citrate: low/normal citrate and CaOx stones, 2-4mEq/kg/d
- Thiola: prevent disulfide bridge formation
- Allopurinol: hyperuricemia + hyperuricosuria, 4-10mg/kg/d (max 300mg/d), treat uric acid stones with hydration and alkalinization
- Pyridoxine: primary hypoxaluria Type 1, 2-5mg/kg/d and titrate up
Surgical management
- Up to 60% will require surgery
- Success rates: 70-97% PCNL, 85-88% URS, 80-83% ESWL
- URS: ureteral stones or renal stones < 2cm
- ESWL: renal stones < 1.5cm, increased need for retreatment if longer infundibulum or infundibulopelvic angle > 45 degrees
- PCNL: renal stones > 2cm
- Similar risks to adult stone surgery, may have higher need for pre-stenting due to narrow ureters
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Carnes, Kevin, et al. "24-Hour urine collection for first time pediatric stone formers: Is it worth it?." Journal of Pediatric Urology 17.3 (2021): 387-e1.
- Puttmann, Kathleen, Daniel Dajusta, and Alexandra W. Rehfuss. "Does twinkle artifact truly represent a kidney stone on renal ultrasound?." Journal of Pediatric Urology 17.4 (2021): 475-e1.
- Tasian, G. and L. Copelovitch. "Management of Pediatric Kidney Stone Disease." Campbell-Walsh Urology 12 (2020).