Posterior Urethral Valves and other Urethral Abnormalities
Pathophysiology
- Bladder outlet obstruction during development leads to downstream effects
- Bladder becomes hypertrophied to compensate for obstruction but empties well with some reflux
- Polyuria from renal dysplasia and glomerular damage leads to incomplete bladder emptying, leading to further reflux and renal damage
- Natural course: detrusor hyperreflexia in infancy -> improved compliance in childhood -> increased capacity with hypocontractility in adolescence (myogenic failure)
- Valve bladder syndrome: caused by polyuria, bladder insensitivity, elevated post-void residuals
Diagnosis
- Prenatal US findings: thickened dilated bladder, bilateral hydroureter/nephrosis, oligohydramnios, dilated posterior urethra (keyhole sign)
- 50% diagnosed prenatally, 25% diagnosed as neonates, 25% diagnosed after presenting with UTI
- Postnatal US findings: thickened distended bladder, possible diverticula, dilated posterior urethra, high bladder neck with hyperplasia, dilated ureters, dysplastic kidneys, possible urinoma
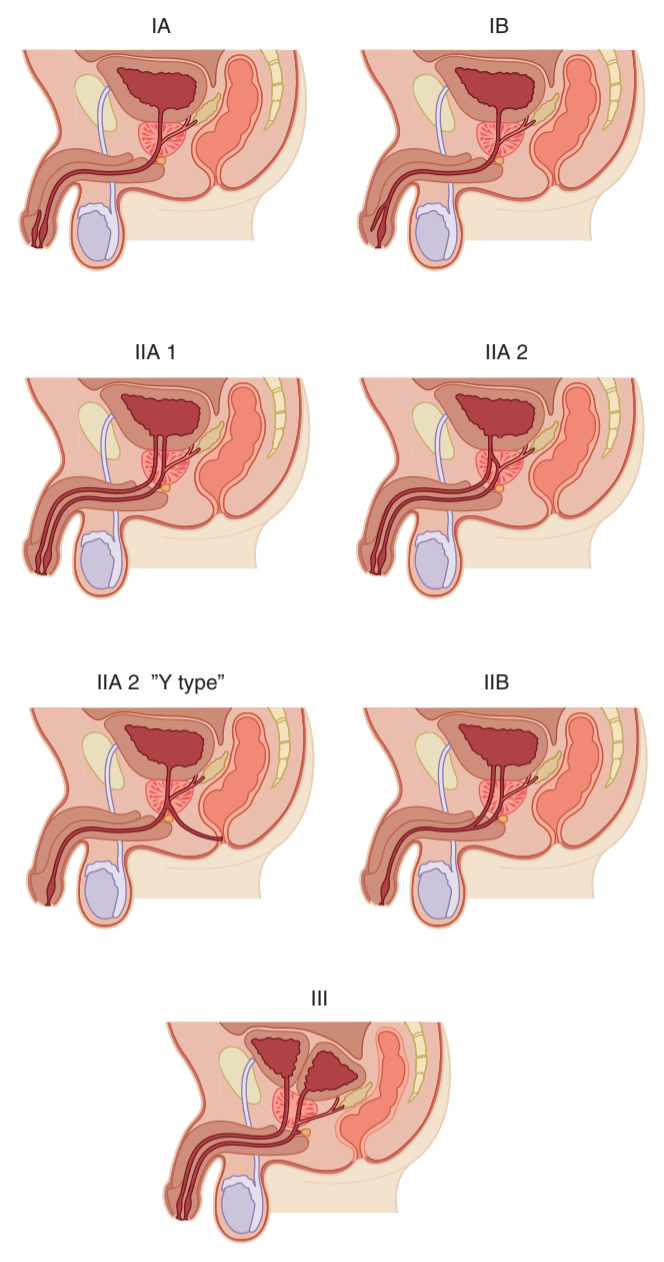
- VCUG findings (definitive test): dilated posterior urethra, bladder neck hypertrophy, dilated ejaculatory ducts, thickened/trabeculated bladder with diverticula, 50% have vesicoureteral reflux, abrupt urethral funneling (obstructing leaflets) - may require coude catheter
Initial management
- No clear benefit to vesicoamniotic shunting
- PLUTO trial: vesicoamniotic shunt vs conservative managment, poor accrual, only 2 children survived to 2yo, intervention increases risk for pregnancy loss
- Catheter (5-7Fr feeding tube) should be placed to optimize urinary drainage, avoid filling balloon to prevent bladder spasms
- Pulmonary hypoplasia is most concerning cause of perinatal mortality
- Urinoma drainage: required infrequently, only if causing respiratory distress or severe abdominal distension
- Valve ablation: performed with direct visualization with Bugbee at 5 + 7 or 12 o'clock, catheter left for 24+hrs
- Vesicostomy: reserved for infants unable to undergo endoscopy due to size/prematurity or continued upper tract deterioration despite valve ablation
- Upper tract diversion: rarely indicated
- Circumcision: recommended to reduce UTI risk, perform prior to considering reimplantation
- VUR: 25-40% resolve with ablation or vesicostomy alone
Long term management
- Repeat VCUG 2-3mo after valve ablation, trend renal appearance with regular ultrasounds
- Obtain uroflow and check PVR to screen for valve bladder syndrome (myogenic failure)
- Daytime incontinence 7-35%, enuresis 25%
- Do not push toilet training, then encourage double/timed voiding and adequate fluid intake
- Consider CIC, can start early to familiarize the child/family
- Can consider a-blockers or anticholinergics but no clear recommendations
- Nocturnal drainage (catheterization) recommended if worsening upper tract dilation, renal function, or UTIs
- Reflux: keep on prophylaxis until reflux resolves, surgical repair high risk for failure due to high pressure bladders
- APV: can consider if nocturnal catheterization difficult due to bladder neck hypertrophy or sensate urethra
- Renal problems: polyuria due to inability to concentrate urine, salt-loss nephropathy due to renal injury, metabolic acidosis, osteodystrophy, and growth issues
- ESRD: occurs in 20-50%, low risk if creatinine < 0.8 and high risk if > 1.2 at 1yo
- Transplant: potential option, but higher risk for failure due to poor bladder function
Anterior urethral valves
- Less common than posterior valves (25-30x)
- Present with postvoid dribbling, penile bulging, palpable bladder, renal insufficiency, UTIs
- VCUG confirms diagnosis with dilated anterior urethra
- Management: valve ablation
- Prognosis: 78% have normal renal function after treatment
Other urethral abnormalities
- Congenital fistula: can be associated with chordee or imperforate anus
- Urethral duplication: rare (200 cases), usually dorsal urethra is accessory, associated with GI/GU abnormalities, assess with RUG/VCUG + cystoscopy
- Urethral atresia: usually incompatible with life unless patent urachus, can treat with vesicostomy
- Urethrorrhagia: blood spotting after urination, usually benign and self-resolving, usualy peripubertal, cystoscopy not recommended (high risk for stricture development)
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Martin, A. and C. Roth. "Bladder Anomalies in Children." Campbell-Walsh Urology 12 (2020).
- Palmer, L., and J. Palmer. "Management of Abnormalities of the External Genitalia in Boys." Campbell-Walsh Urology 12 (2020).