Lower Tract Abnormalities
Bladder Abnormalities
Developmental anomalies
- Prenatal bladder normally visible in 50% by 10 weeks, 100% by 13 weeks
- Bladder agenesis: can only be diagnosed after 15-20 minutes visualization to make sure bladder is not just empty, compatible with life only if ureters drain into mullerian structures (female) or rectum (male), treat with ureterosigmoidostomy
- Megacystis: prenatally dilated bladder, spontaneously resolves if no obstructive uropathy and normal karyotype
- Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS): presents prenatally with distended bladder, presents postnatally with abdominal distension and inability to pass meconium, managed with ileostomy + Gtube + TPN, may require small intestine transplant, most will require CIC +/- vesicostomy
- Duplication: can be complete or incomplete, 90% have external genital abnormalities, 42% have GI abnormalities, goals are removing obstruction and preserving renal function
Bladder diverticula
- VCUG provides best imaging to confirm diagnosis
- Primary Hutch: otherwise smooth-walled bladder, no other diverticula, no evidence obstruction
- Secondary Hutch: other diverticula present in trabeculated bladder, caused by infravesical obstruction
- Asymptomatic diverticula can be treated conservatively
- Surgical intervention warranted if VUR, stones, UTI
Acquired bladder conditions
- Hemangiomas: seen with syndromes, may cause hematuria/dysuria, manage with biopsy/fulguration or partial cystectomy (if large)
- Polyps: may present with hematuria/dysuria or obstruction, manage with resection
- Nephrogenic adenoma: manage with resection, 80% recurrence rates
- Eosinophilic cystitis: present with hematuria/dysuria, retention, and SP pain, biopsy shows eosinophils throughout specimen, manage with combination of steroids + antihistamines + antibiotics once diagnosed via biopsy
- Hemorrhagic cystitis: related to either cyclophosphamide/ifosfamide, viral infection, or radiation
Urachal anomalies
- Patent urachus: urachal canal fails to obliterate, only 14% have some form of bladder obstruction, may have persistent drainage via umbilicus, diagnose with fistulogram or VCUG, drain if infected
- Urachal sinus: obliterated at bladder but open to umbilicus, diagnose with fistulogram (negative VCUG findings)
- Urachal cyst: no clear communication with bladder/umbilicus, but may drain intermittently, can become infected, diagnose with US/CT/MR
- Urachal diverticulum: urachus obliterates except at bladder apex, may cause stones or UTI
- Management: urachal remnant should be completely excised, include bladder cuff if attached

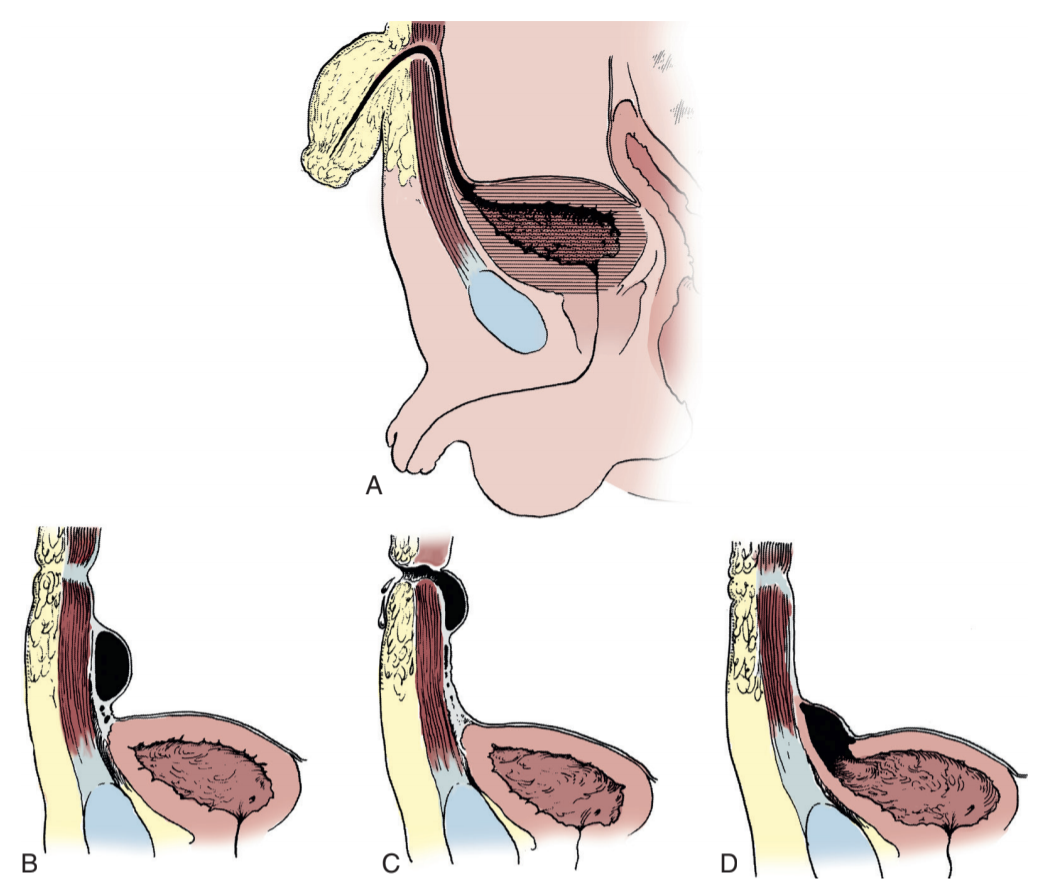
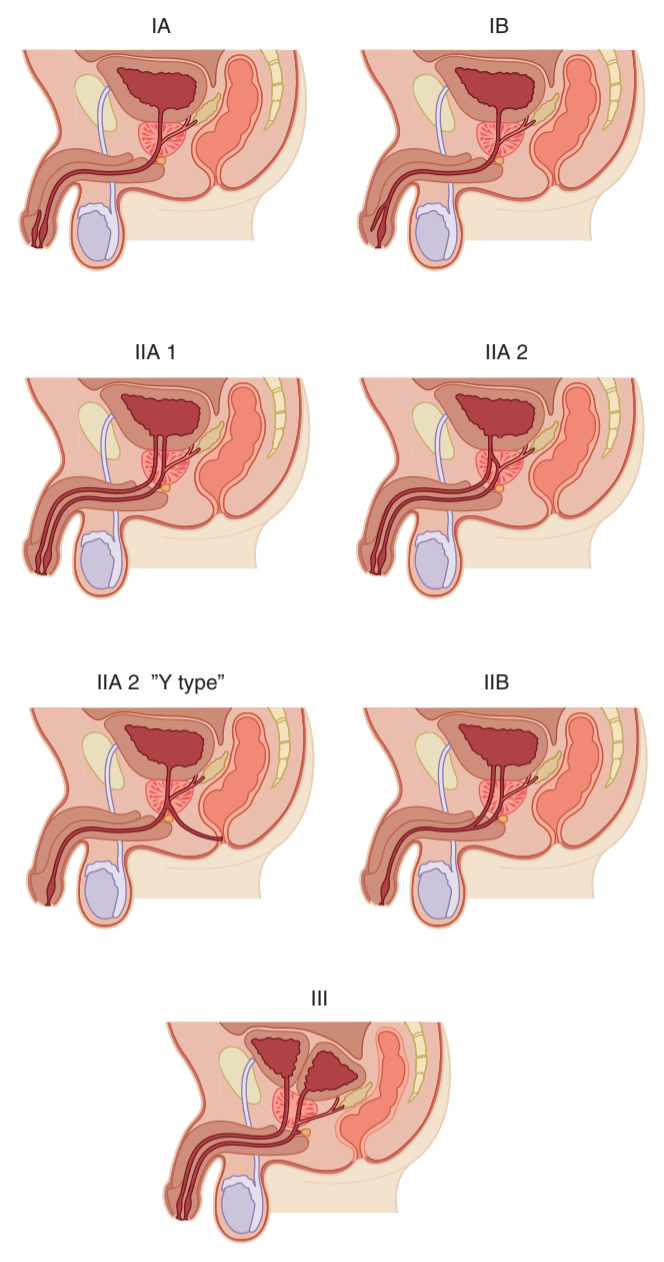
Exstrophy reconstruction timeline, from Campbell's
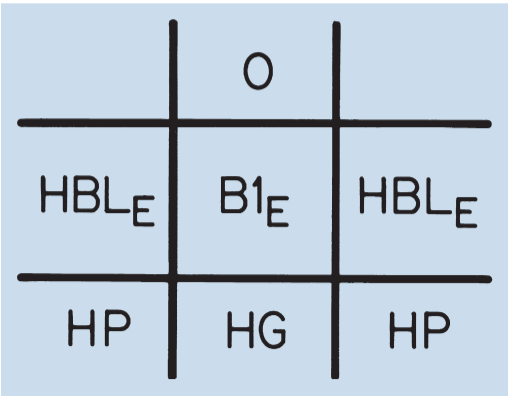
Cloacal exstrophy grid for descriptions - O (omphalocele), B1 (bowel), HBL (hemibladder), HG (hindgut), HP (hemiphallus) - from Campbell's
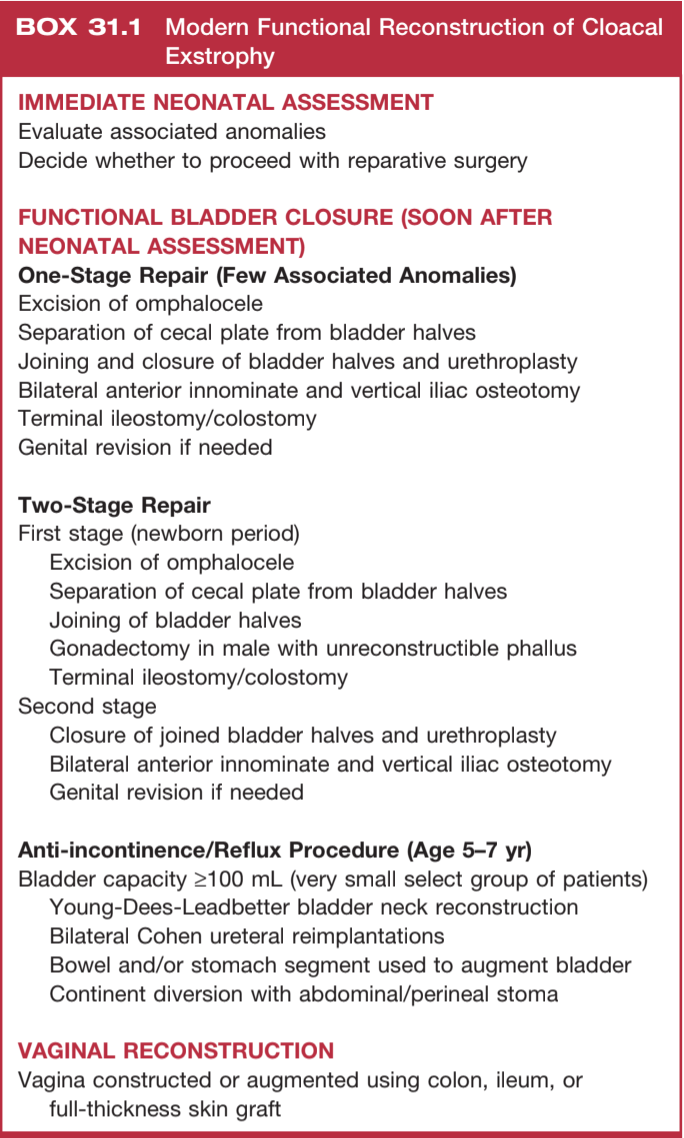
Cloacal exstrophy reconstruction, from Campbell's
Exstrophy/Epispadias Complex
Epidemiology and Prenatal Diagnosis
- Incidence: 2.15 per 100K live births
- If prior child with bladder exstrophy, chances of future child are 1:100
- Chances of patient with exstrophy having a child with exstrophy: 1:70
- Prenatal US: may note absence of bladder filling, low-set umbilicus, widened pubic ramus, small genitals, and lower abdominal mass
- Neonatal evaluation: obtain renal US to assess for hydronephrosis, pelvic XR to assess pubic diastasis, and spinal US to assess for spina bifida
Bladder considerations
- Bladder mucosa should be immediately protected with membrane to prevent metaplastic changes
- Bladder neds to be examined under anesthesia to adequately assess depth of bladder extension
- Reflux will always happen in closed bladder and reimplantation is required
Genital considerations
- Corpora cavernosa are shorter and wider than normal
- Testes may be retractile but fertility is normal
- Retrograde ejaculation may occur even after bladder neck reconstruction
- Uterine prolapse more common due to poor pelvic floor support
Other considerations
- Workup: check CBC/BMP, renal US (risk for renal anomalies), and KUB (assess pubic diastasis)
- Orthopedic abnormalities result in waddling gait and outward limb rotation
- Levator ani positioned posteriorly and laterally
- Inguinal hernias present in 82% boys and 11% girls
- Anus positioned more anteriorly, 2% incidence of GI anomalies - imperforate anus, rectal stenosis, rectal prolapse
Repair considerations
- Will require bladder closure, abdominal wall closure, posterior urethral closure, osteotomies, epispadias repair, bladder neck reconstruction, and antireflux procedure
- Osteotomy goals: relaxing tension on GU repairs
- Primary closure: maintain adequate bladder and ureteral drainage
- If primary repair attempts fail, can consider ureterosigmoidostomy or complete urinary diversion
Repair complications
- Penile ischemia: due to corporal injury, more common if osteotomies not performed
- Urethrocutaneous fistula: seen in 5-40%, may spontaneously close if SPT placed, if not may require repeat reconstruction
- Dehiscence: uncommon, may occur with bladder or abdominal wall, requires redo reconstruction
- Urethral obstruction: evaluate with cystoscopy, may require SPT or CIC
- Epididymitis: 19-33%, evaluate for high pressure voiding and strictures
- Malignancy: adenocarcinoma most common, increased risk if colon used for augment
- MSK: increased risk for gait abnormalities and hip/pelvic pain later in life
Longterm issues (into adulthood)
- UTI: common, exacerbated by presence of VUR, can cause longterm renal injury
- Male genital: phallus size/appearance, difficulty with penetration, difficulty with condom sizing, management may require specialized center referrals
- Female genital: increases risk for pelvic prolapse (onset at younger age than general population), C-section recommended
- Urinary: increased risk for stress incontinence after outlet surgery (high dependence on bladder neck for baseline continence)
Cloacal exstrophy
- Will have features of bladder exstrophy, along with exstrophy of terminal ileum, imperforate anus, and omphalocele
- Spinal abnormalities noted in 85-100%
- Uterine duplication seen in > 90% patients
Eagle Barrett syndrome (Triad, Prune-Belly)
General considerations
- 3 main findings: deficient abdominal muscles, bilateral intraabdominal testes, and urinary tract anomalies (hydronephrosis, renal dysplasia, tortuous ureters, enlarged bladder, dilated prostatic urethra)
- Most important determinant of long-term survival is severity of urinary tract anomalies (especially renal dysplasia)
- Female patients lack gonadal abnormalities
- no clear genetic/embryologic etiology
GU findings
- Renal dysplasia present in 50%
- Vesicoureteral reflux present in 75%
- Urachus present at birth in 25-30%
- Normal voiding, normal flow rates, and normal postvoid residual seen in 50%
- Retrograde ejaculation due to incompetent bladder neck
- Urethral atresia common, lethal unless patent urachus
- Most severely affected abdominal wall may consist solely of skin, subQ fat, and fibrous preperitoneal layer
Non-GU findings
- Seen in 75%, mainly cardiac, pulmonary, orthopedic
- Up to 10% cardiac anomalies - patent ductus arteriosus, ASD/VSD, tetralogy of Fallot
- Higher risk for respiratory infections due to inability to generate significant intraabdominal pressure
- Up to 30% GI anomalies - incomplete rotation, imperforate anus, lifelong constipation
- Up to 65% orthopedic anomalies - clubfoot (26%), hip dysplasia (5%), scoliosis (4%)
Presentation/Diagnosis
- Prenatal US at ~30 weeks may see hydronephrosis, distended bladder, irregular abdominal circumference
- Category I: severe pulmonary hypoplasia and skeletal abnormalities
- Category II: non-prominent pulmonary hypoplasia, usually renal insufficiency and hydronephrosis
- Category III: mild/incomplete features, no pulmonary hypoplasia
- Incomplete: unilateral abdominal wall deficiency and unilateral undescended testis, risk for ernal insufficiency
- Adult presentation: if lacking abdominal wall features, may present with renal failure and HTN, UTIs due to chronic urinary stasis
- Attempt to maintain creatinine < 0.7, predictive of good renal function
Management
- Prenatal intervention warranted if concern for urethral atresia with oligohydramnios, otherwise lethal
- Circumcision recommended to minimize UTI risks
- Obtain renal US for baseline assessment of renal parenchyma
- VCUG assesses BOO and VUR
- Antibiotic prophylaxis required for any GU instrumentation
- Upper tract surgeries: vesicostomy, ureteroplasty, ureterocystoneostomy
- Lower tract surgeries: reduction cystoplasty, internal urethrotomy, urethroplasty
- Genital surgeries: orchiopexy
- Abdominal wall: reconstruction warranted for cosmetic or functional benefits
- Category I: supportive care only, minimal/no benefit to interventions
- Category II: individualized interventions based on severity
- Category III: regular renal US and BMP, correct cryptorchidism and VUR
Posterior Urethral Valves and other Urethral Abnormalities
Pathophysiology
- Bladder outlet obstruction during development leads to downstream effects
- Bladder becomes hypertrophied to compensate for obstruction but empties well with some reflux
- Polyuria from renal dysplasia and glomerular damage leads to incomplete bladder emptying, leading to further reflux and renal damage
- Natural course: detrusor hyperreflexia in infancy -> improved compliance in childhood -> increased capacity with hypocontractility in adolescence (myogenic failure)
- Valve bladder syndrome: caused by polyuria, bladder insensitivity, elevated post-void residuals
Diagnosis
- Prenatal US findings: thickened dilated bladder, bilateral hydroureter/nephrosis, oligohydramnios, dilated posterior urethra (keyhole sign)
- 50% diagnosed prenatally, 25% diagnosed as neonates, 25% diagnosed after presenting with UTI
- Postnatal US findings: thickened distended bladder, possible diverticula, dilated posterior urethra, high bladder neck with hyperplasia, dilated ureters, dysplastic kidneys, possible urinoma
- VCUG findings (definitive test): dilated posterior urethra, bladder neck hypertrophy, dilated ejaculatory ducts, thickened/trabeculated bladder with diverticula, 50% have vesicoureteral reflux, abrupt urethral funneling (obstructing leaflets) - may require coude catheter
Initial management
- No clear benefit to vesicoamniotic shunting
- PLUTO trial: vesicoamniotic shunt vs conservative managment, poor accrual, only 2 children survived to 2yo, intervention increases risk for pregnancy loss
- Catheter (5-7Fr feeding tube) should be placed to optimize urinary drainage, avoid filling balloon to prevent bladder spasms
- Pulmonary hypoplasia is most concerning cause of perinatal mortality
- Urinoma drainage: required infrequently, only if causing respiratory distress or severe abdominal distension
- Valve ablation: performed with direct visualization with Bugbee at 5 + 7 or 12 o'clock, catheter left for 24+hrs
- Vesicostomy: reserved for infants unable to undergo endoscopy due to size/prematurity or continued upper tract deterioration despite valve ablation
- Upper tract diversion: rarely indicated
- Circumcision: recommended to reduce UTI risk, perform prior to considering reimplantation
- VUR: 25-40% resolve with ablation or vesicostomy alone
Long term management
- Repeat VCUG 2-3mo after valve ablation, trend renal appearance with regular ultrasounds
- Obtain uroflow and check PVR to screen for valve bladder syndrome (myogenic failure)
- Daytime incontinence 7-35%, enuresis 25%
- Do not push toilet training, then encourage double/timed voiding and adequate fluid intake
- Consider CIC, can start early to familiarize the child/family
- Can consider a-blockers or anticholinergics but no clear recommendations
- Nocturnal drainage (catheterization) recommended if worsening upper tract dilation, renal function, or UTIs
- Reflux: keep on prophylaxis until reflux resolves, surgical repair high risk for failure due to high pressure bladders
- APV: can consider if nocturnal catheterization difficult due to bladder neck hypertrophy or sensate urethra
- Renal problems: polyuria due to inability to concentrate urine, salt-loss nephropathy due to renal injury, metabolic acidosis, osteodystrophy, and growth issues
- ESRD: occurs in 20-50%, low risk if creatinine < 0.8 and high risk if > 1.2 at 1yo
- Transplant: potential option, but higher risk for failure due to poor bladder function
Anterior urethral valves
- Less common than posterior valves (25-30x)
- Present with postvoid dribbling, penile bulging, palpable bladder, renal insufficiency, UTIs
- VCUG confirms diagnosis with dilated anterior urethra
- Management: valve ablation
- Prognosis: 78% have normal renal function after treatment
Other urethral abnormalities
- Congenital fistula: can be associated with chordee or imperforate anus
- Urethral duplication: rare (200 cases), usually dorsal urethra is accessory, associated with GI/GU abnormalities, assess with RUG/VCUG + cystoscopy
- Urethral atresia: usually incompatible with life unless patent urachus, can treat with vesicostomy
- Urethrorrhagia: blood spotting after urination, usually benign and self-resolving, usualy peripubertal, cystoscopy not recommended (high risk for stricture development)
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Denes, F. and R. Lopes. "Prune-Belly Syndrome." Campbell-Walsh Urology 12 (2020).
- Gearhart, J. and H. DiCarlo. "Exstrophy-Epispadias Complex." Campbell-Walsh Urology 12 (2020).
- Martin, A. and C. Roth. "Bladder Anomalies in Children." Campbell-Walsh Urology 12 (2020).
- Palmer, L., and J. Palmer. "Management of Abnormalities of the External Genitalia in Boys." Campbell-Walsh Urology 12 (2020).