Female Genital Abnormalities
Vestibular anomalies
- Urethral prolapse: presents with underwear spotting, visible as doughnut-shaped mass with meatus at center, manage with topical steroids/estrogens, excision, or sitz baths, non-surgical management has 67% recurrence rates
- Urethral polyp: rare interlabial mass, treat with excision
- Paraurethral cyst: originate from Skene duct, displace urethral meatus with abnormal urinary stream, can perform needle drainage (otherwise resolve spontaneously)
- Mesonephric duct remnant: originate from Gartner duct (incomplete Wolffian duct regression), may have ectopic ureteral drainage, can inject contrast retrograde to assess anatomy, may require heminephrectomy if severely dysplastic or nonfunctional
- Prolapsed ureterocele: may prolapse via urethra during urination, diagnose with exam and renal US, manage with needle decompression or incision, then catheter placement
- Ectopic ureter: may insert distal to urethral sphincter, causes diurnal incontinence with otherwise normal void pattern
Vaginal anomalies
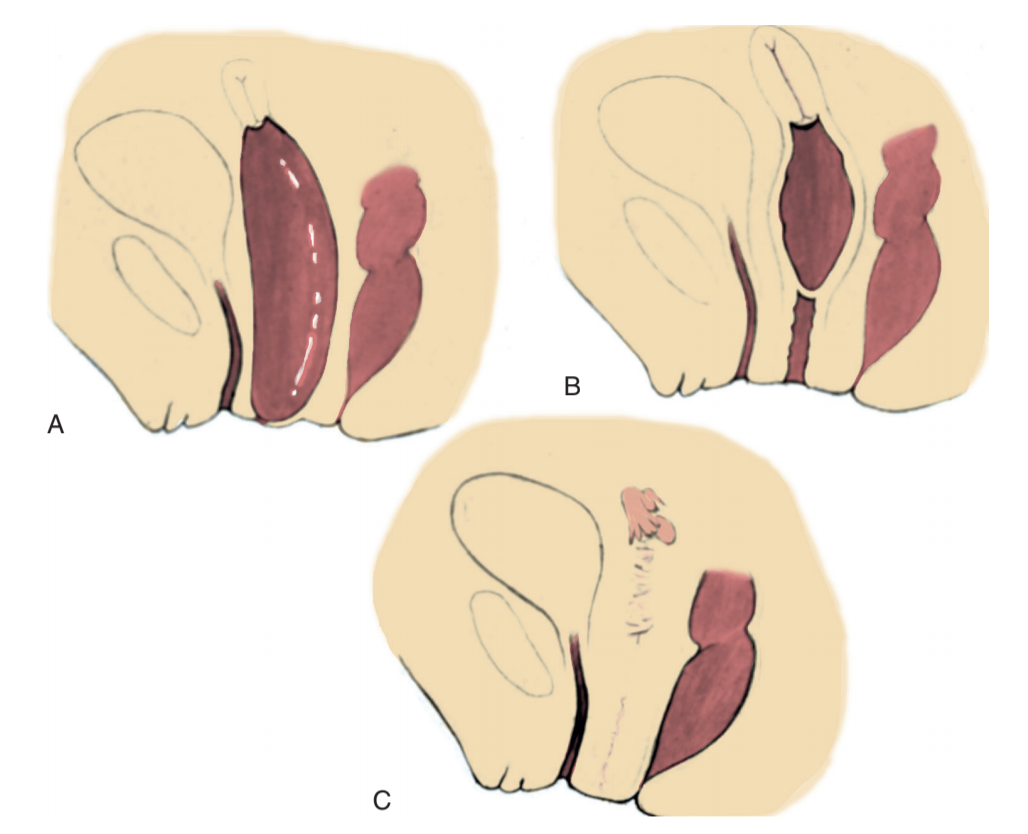
- Imperforate hymen: may be diagnosed at birth (retained fluid) or during adolecence (amenorrhea + cyclic abdominal pain), identify bluish bulging hymen, treat with transverse incision in neonate, excise under anesthesia in teenager
- Imperforate hymen: failure of urogenital sinus and mullerian ducts to fuse/canalize, presents with amenorrhea + distended upper vagina, MR helpful to determine presence/absence of cervix, can delay surgery with hormonal suppression of menstrual cycle, definitive management with surgical repair
- Vaginal atresia: urogenital sinus fails to form distal vagina, normal mullerian structures (not present in AIS), presents with shallow vaginal dimple, manage with pull-through surgery and skin flaps
- Vaginal agenesis / Mullerian aplasia / MRKH syndrome: absent proximal vagina +/- uterus in otherwise normal (phenotypic/chromosomal/hormonal) female, 1/3 have urinary abnormalities
- Cervical atresia: can be managed with anastomosis of vaginal remnant to uterus with subsequent pregnancy (managed with C-section), but risk for ascending infections
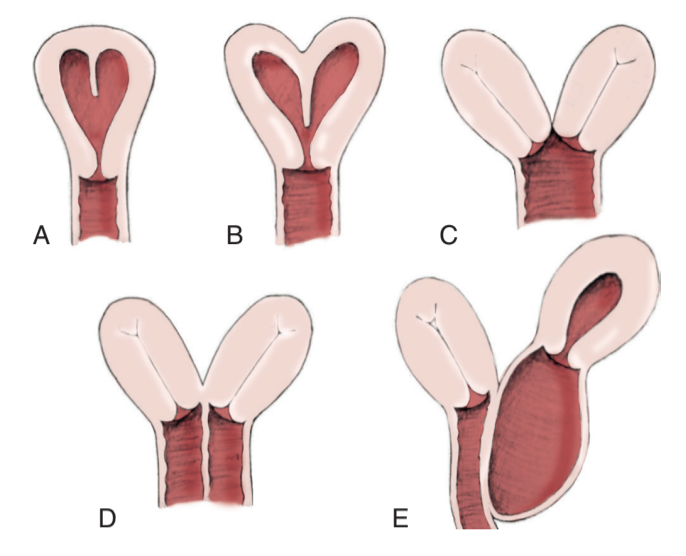
Lateral fusion abnormalities
- Uterine didelphys: two separate uteri and cervices
- Duplication with unilateral imperforate vagina (Herlyn Werner Wunderlich syndrome): rare, cyclic abdominal pain with normal menses, lateral bluish vaginal bulge, may have complete or incomplete obstruction, manage with incision of vaginal septum
Neovagina tips
- Goals: ability to achieve intercourse, able to use largest dilator without discomfort, or vaginal length > 7cm - achieved with vaginal dilation + perineal pressure
- Tissue: create from skin, intestine, muscle flaps, or labia majora
- Important to have patient talk to someone who previously underwent procedure
Acquired disorders of female genitalia
- Labial adhesions: seen in 0.6-1.8%, occurs posteriorly and advances towards clitoris, spontaneously resolve in 80% within 1yr, otherwise can treat with topical estrogen and traction or surgical revision
- Female circumcision: no medical indication, can result in chronic pain +/- UTI +/- dyspareunia +/- fistula, severity ranges from clitoral excision to complete obstruction of vestibule
- Inguinal hernia: 1% chance of cAIS, vaginoscopy to assess cervical presence/absence is more cost effective than pelvic US or karyotype, can also perform inguinal laparoscopy - round ligament and mullerian structures will be absent in genetic males
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Kaefer, M. "Management of Abnormalities of the Genitalia in Girls." Campbell-Walsh Urology 12 (2020).