Bowel Dysfunction
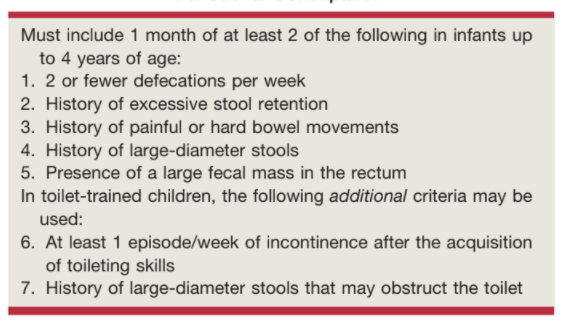
Rome IV Criteria for Functional Constipation, from Campbell's
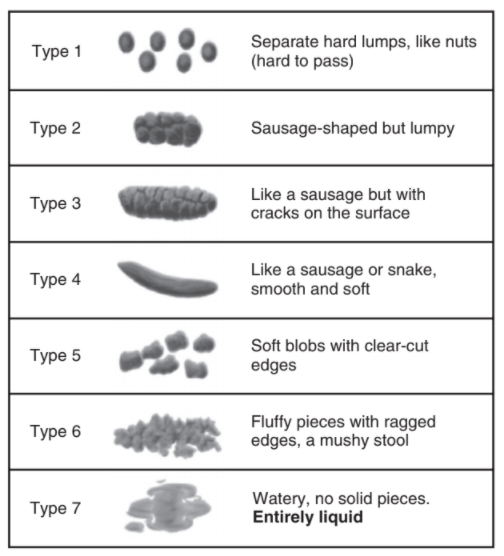
Bristol Stool Scale, from Campbell's
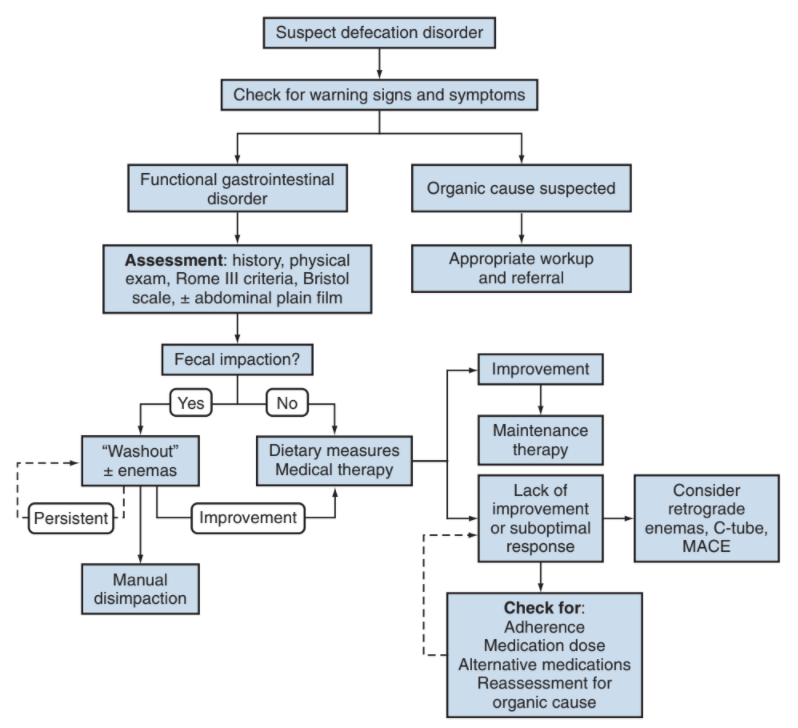
Constipation algorithm, from Campbell's
Bowel Dysfunction
General considerations- Voluntary control expected by age 3
- Majority have daily BM without straining, ranges from 3x daily to every 3 days
- Functional constipation prevalence: 0.7-29.6%
Evaluation
- HPI: age of onset, inability to toilet train, BM frequency and consistency, growth patterns
- Prior surgeries: GI, GU, and pelvic
- Exam: sacral anomalies, abdominal masses, normal neurologic function
- DRE: not indicated
- KUB: may be helpful to assess stool burden but not required
Management
- Behavioral: increased fluids/fiber, post-meal BMs, flexing thighs to abdomen to optimize abdominal pressure
- Wash-out: miralax 1-1.5 g/kg/day or mineral oil enemas for 3-6 days
- For complex cases, may require NGT + IVF, possible disimpaction under anesthesia
- Miralax maintenance: 0.2-0.8 g/kg/day, titrate up as needed
- Malone antegrade continence enema (MACE): allows for complete colonic emptying for continence, via continent cutaneous bowel access, may allow for greater patient independence
References
- AUA Core Curriculum`
- Austin, P. and A. Seth. "Functional Disorders of the Lower Urinary Tract in Children." Campbell-Walsh Urology 12 (2020).
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Koyle, M. and A. Lorenzo. "Management of Defecation Disorders." Campbell-Walsh Urology 12 (2020).