Bladder Abnormalities
Developmental anomalies
- Prenatal bladder normally visible in 50% by 10 weeks, 100% by 13 weeks
- Bladder agenesis: can only be diagnosed after 15-20 minutes visualization to make sure bladder is not just empty, compatible with life only if ureters drain into mullerian structures (female) or rectum (male), treat with ureterosigmoidostomy
- Megacystis: prenatally dilated bladder, spontaneously resolves if no obstructive uropathy and normal karyotype
- Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS): presents prenatally with distended bladder, presents postnatally with abdominal distension and inability to pass meconium, managed with ileostomy + Gtube + TPN, may require small intestine transplant, most will require CIC +/- vesicostomy
- Duplication: can be complete or incomplete, 90% have external genital abnormalities, 42% have GI abnormalities, goals are removing obstruction and preserving renal function
Bladder diverticula
- VCUG provides best imaging to confirm diagnosis
- Primary Hutch: otherwise smooth-walled bladder, no other diverticula, no evidence obstruction
- Secondary Hutch: other diverticula present in trabeculated bladder, caused by infravesical obstruction
- Asymptomatic diverticula can be treated conservatively
- Surgical intervention warranted if VUR, stones, UTI
Acquired bladder conditions
- Hemangiomas: seen with syndromes, may cause hematuria/dysuria, manage with biopsy/fulguration or partial cystectomy (if large)
- Polyps: may present with hematuria/dysuria or obstruction, manage with resection
- Nephrogenic adenoma: manage with resection, 80% recurrence rates
- Eosinophilic cystitis: present with hematuria/dysuria, retention, and SP pain, biopsy shows eosinophils throughout specimen, manage with combination of steroids + antihistamines + antibiotics once diagnosed via biopsy
- Hemorrhagic cystitis: related to either cyclophosphamide/ifosfamide, viral infection, or radiation
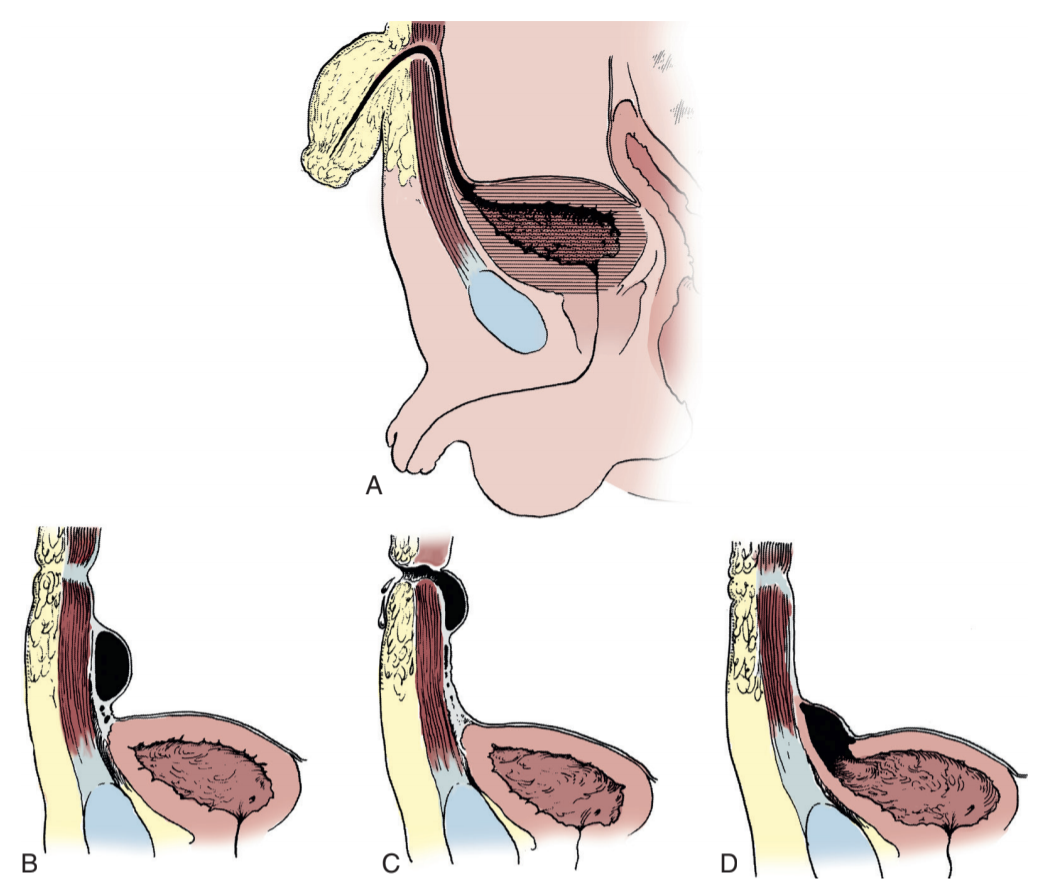
Urachal anomalies
- Patent urachus: urachal canal fails to obliterate, only 14% have some form of bladder obstruction, may have persistent drainage via umbilicus, diagnose with fistulogram or VCUG, drain if infected
- Urachal sinus: obliterated at bladder but open to umbilicus, diagnose with fistulogram (negative VCUG findings)
- Urachal cyst: no clear communication with bladder/umbilicus, but may drain intermittently, can become infected, diagnose with US/CT/MR
- Urachal diverticulum: urachus obliterates except at bladder apex, may cause stones or UTI
- Management: urachal remnant should be completely excised, include bladder cuff if attached
References
- AUA Core Curriculum
- Baskin, Laurence S. Handbook of pediatric urology. Lippincott Williams & Wilkins, 2018.
- Martin, A. and C. Roth. "Bladder Anomalies in Children." Campbell-Walsh Urology 12 (2020).