Penile Cancer
Pre-Cancerous/Malignant Lesions
Penile Intraepithelial Neoplasia (PEIN/PIN)
- Associated with HPV in 90% cases
- Erythroplasia of Queyrat: CiS of glans or prepuce, progression in 10-33%
- Bowen disease: CiS of penile shaft, genitalia, or perineal region, progression in 5%
- Bowenoid papulosis: similar-appearing to CiS but benign, multiple papules
- Treatment: topical options (5-FU, 5% imiquimod), laser excision, circumcision (if located on foreskin), 5mm margin usually adequate for local control
Balanitis Xerotica Obliterans (BXO, male lichen sclerosis)
- Appearance: whitish patches on prepuce/glans/meatus/fossa navicularis
- Treatment: clobetasol cream for 2-3 months, treat urethral stenosis with dilation, steroids, and/or reconstruction
Condyloma acuminata (genital warts)
- Rare before puberty (potentially indicates sexual abuse)
- Urethral involvement: seen in 5%, may require 5-FU, pediatric resectoscope, or urethroplasty
- HPV: present in 50-70% specimens, risk increased with uncircumcised state, increased sexual partners, non-condom use, and smoking
- Subclinical lesions: diagnosed via applying 5% acetic acid, lesions will be white under magnifying glass
- Treatments: trichloroacetic acid 35-85%, cryotherapy, electrofulguration, CO2 laser, imiquimod 5% cream
- Circumcision: consider removing preputial lesions and provide better glans exposure
Buschke-Lowenstein Tumor
- Definition: uncontrolled local growth of condylomas causing destruction/displacement of adjacent tissues without metastasis
- Diagnosis: excisional or deep biopsies required to differentiate from penile cancer
- Treatment: complete excision and possible skin grafts, XRT and topical therapies non-beneficial
Kaposi Sarcoma
- Varieties: classic (indolent), immunosuppressive, African (young, indolent or aggressive), epidemic or HIV-related
- Treat nonepidemic forms aggressively due to rarity of diffuse organ involvement, usually surgery/XRT effective
- Consider withdrawing immunosuppression to treat
- AIDS: increases risk x7000, can treat with surgery, XRT, or laser removal
Penile Cancer
Risk Factors
- Neonatal circumcision: almost completely eliminates risk, no proven benefit for adult circumcision
- HPV seen in 31-63% penile cancers
- Other risk factors: HIV, tobacco use, increased sexual partners, trauma, BXO, UV exposure (psoriasis treatment)
- Not risk factors: smegma, topical carcinogens (cause scrotal cancer), STDs (besides HPV)
Natural History
- Stepwise spread: sentinel node, superficial inguinal nodes, deep inguinal nodes, pelvic nodes, distant metastasis
- Local spread: invasion through Buck fascia can lead to vascular dissemination of tumor
- Regional nodal metastases: untreated leads to skin necrosis, infection, hemorrhage from erosion into femoral vessels
- Clinically detectable metastases seen in 1-10%, presence in absence of regional nodal metastases is rare, most common sites lung, liver, bone, brain
- Mortality: high within 2 years, no spontaneous remission reported, second primary develops in 5-17%
Presentation
- Penile lesion: first sign, according to Campbell's may present as a "luxuriant exophytic lesion"
- Phimosis can obscure a lesion, presenting with erosion through prepuce, odor, discharge/bleeding
- Location: glans (48%), prepuce (21%), prepuce + glans (9%), coronal sulcus (6%), shaft (< 2%)
- Pain not a common symptom
- Inguinal lymph node exam: important, more informative than imaging, but can understage in 10% and overstage in 16%
- Staging imaging: although exam more accurate, CT/MR beneficial in obese patients
- Care delays: > 1yr in 15-50%, high levels of denial regarding condition
- Biopsy: assess depth, vascular invasion, and histologic grade, can perform prior to definitive surgical treatment
- Low-grade lesions make up 70-80% cases
Imaging indications
- Metastatic workup: evaluate C/A/P + CMP if palpable nodes, at risk for inguinal spread, or proven inguinal spread, consider bone scan if bone pain or elevated AlkPhos
- Palpable nodal disease: obtain CT A/P to assess for poor prognostic features - central necrosis or irregular nodal border are predictive of 3+ positive LN, ENE, or positive pelvic nodes
- Organ-sparing: consider penile US/MR to assess for corporal invasion
Findings based on stage/grade
- Inguinal metastases by stage: T1a 10-18%, T1b 33-50%, T2 (33-35%), T3 (49-53%)
- Inguinal metastases by histology: verrucous (none), papillary/warty (low), squamous (low/intermediate), basaloid (intermediate) adenosquamous (intermediate/high), sarcomatoid (high)
- Disease-specific survival by stage: T2 (78%), T3 (53%), N1 (90%), N2 (60%)
- Disease-specific survival by histology verrucous (very high), papillary/warty/adenosquamous (high), squamous/basaloid (intermediate), sarcomatoid (very low)
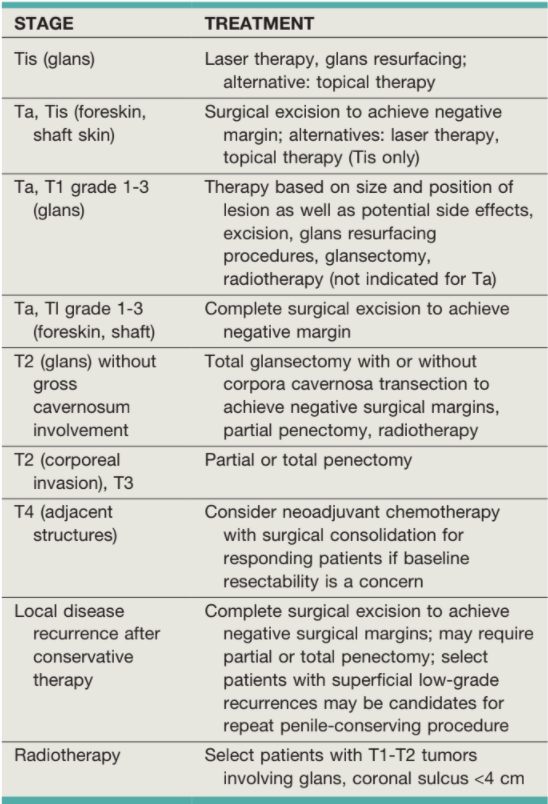
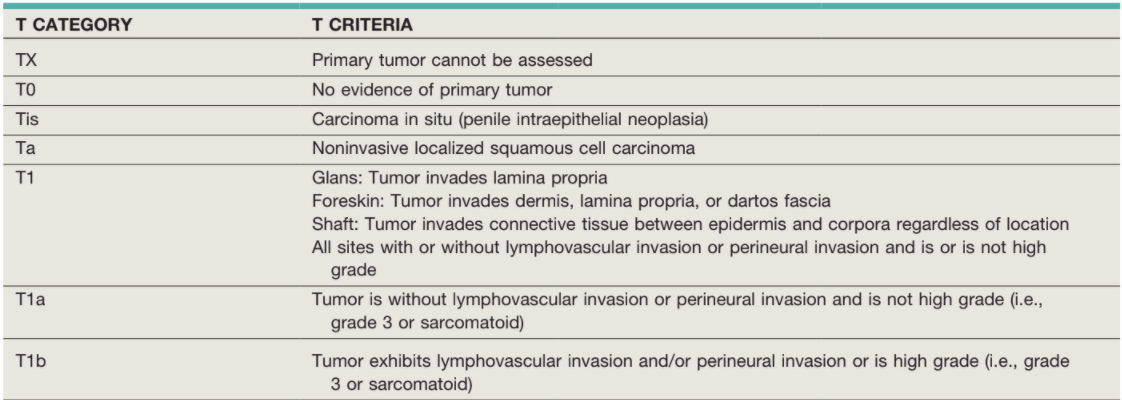
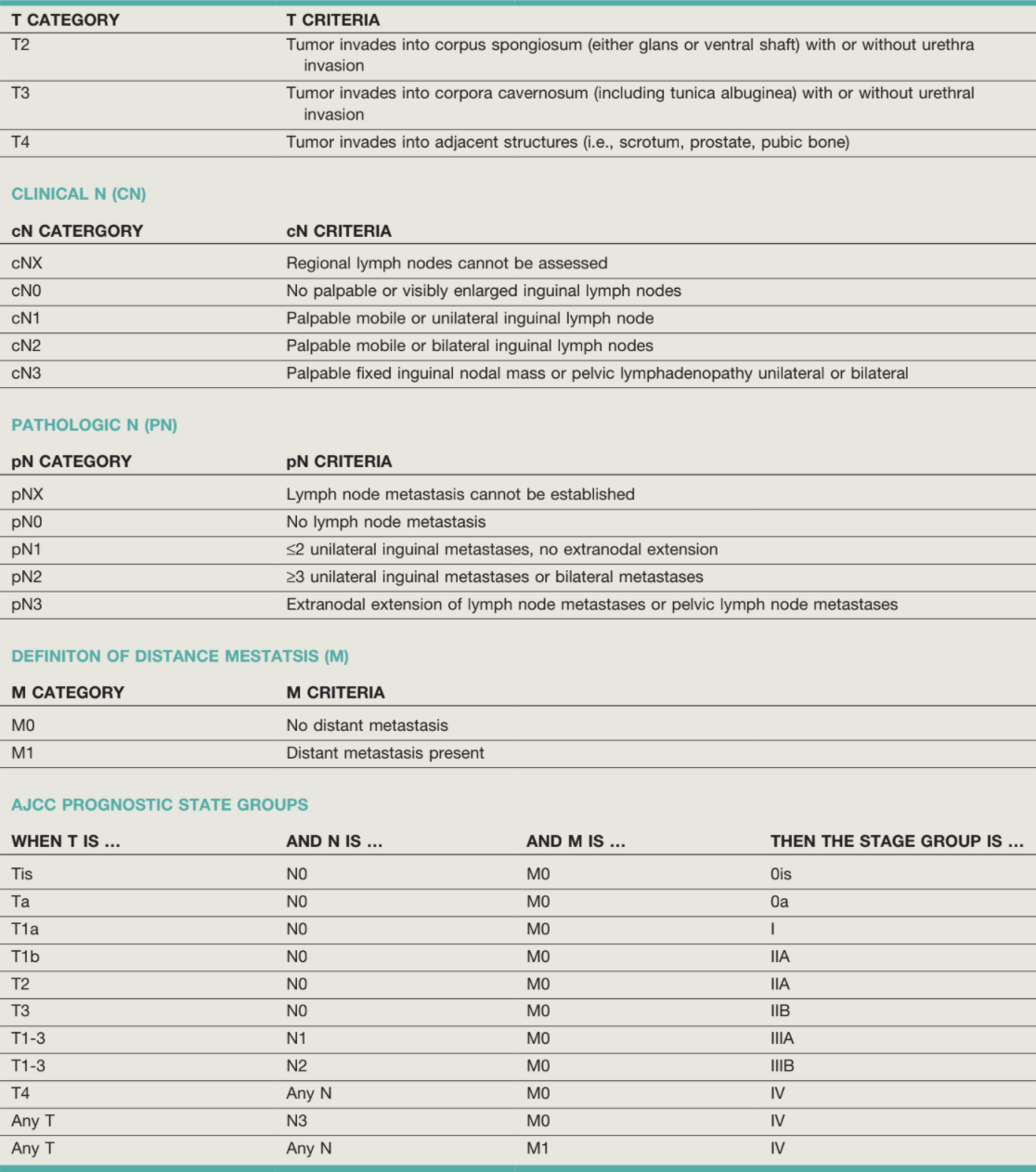
Primary Penile Cancer Treatment Options, Campbell's

Primary Penile Cancer Treatment Algorithm, Campbell's
Penile Cancer Treatments
Surgical options
- Penectomy indications: > 4cm, grade 3-4, or T2+
- Perineal urethrostomy: perform with penectomy, minimize stenosis by spatulating urethra
- Partial penectomy criteria: tumor on glans, prepuce, or distal shaft, patient will be left with adequate length (> 2-3cm) for voiding and intercourse
- Glansectomy: consider if Ta-T2 and limited to glans, does not remove corpora
- Risk of local recurrence: penectomy (0-8%), organ-sparing (2-6%), laser ablation (7-20%), Mohs surgery (32%)
- Palliative resection: may improve short-term QoL but rarely provides cure, survival 21% (1yr), 8% (2yr), 4% (3yr)
Organ-sparing options
- Indications: unable/unwilling to undergo surgery, desire sexual preservation and anatomy
- Organ-sparing criteria: Tis, Ta, or T1 (low grade), able to obtain margins < 2cm
- Minimally invasive options: glans stripping and Mohs surgery, no proven benefit over other options
- Topical therapy (imiquimod, 5-FU): consider for Ta, TiS, local recurrence rates 50%
Radiation
- Criteria: most appropriate if T1-T2, < 4cm, no/minimal extension beyond coronal sulcus
- Indications: too old/sick for surgical therapy, or locoregionally advanced disease
- Primary tumors: may require pre-XRT circumcision (prevents XRT phimosis) and post-XRT salvage surgery
- Results: 5yr local control 55-70%, penile preservation 39-66%
- Worse outcomes: T3+, > 4cm, high grade tumors, recommended to give chemotherapy
- Brachytherapy: 5yr local control 77-88% and penile preservation 74-88%, 10yr local control 70-80% and penile preservation 67-70%
- Side effects: acute desquamation, meatal stenosis (10-45%), soft-tissue ulceration (0-26%), glans necrosis (10-20%), corporal fibrosis
- Inguinal XRT: consider if multiple positive LN or concern for ENE, can consider for multimodal therapy
Chemotherapy
- First-line: TIP (paclitaxel, ifosfamide, cisplatin), preferred for before/after node dissection and for distant metastatic disease
- Up-front indications: T4, fixed nodes (T3), M1
- Adjuvant (after ILND) indications: 3+ nodes, ENE, or pelvic metastases
- Adjuvant benefits: decreases relapse rates (16% vs 45%), but toxicity risk is high
Follow-Up
- Low Risk (Tis, Ta, T1a): physical exam q3m year 1-2, q4m year 3, q6m year 4, q12m year 5+
- High Risk (T1b+): physical exam q2m year 1-2, q3m year 3, q6m year 4, q12m year 5+
- Penile-preserving treatment: q3m year 1-2, q6m year 3
- Partial penectomy: q6m year 1-2, q12m year 3
- ILND with pN0: physical exam q4m year 1-2, q6m year 3, q12m year 4+
- ILND with pN1+: physical exam + CT + CXR q3m year 1-2, q4m year 3, q6m year 4, q12m year 5+
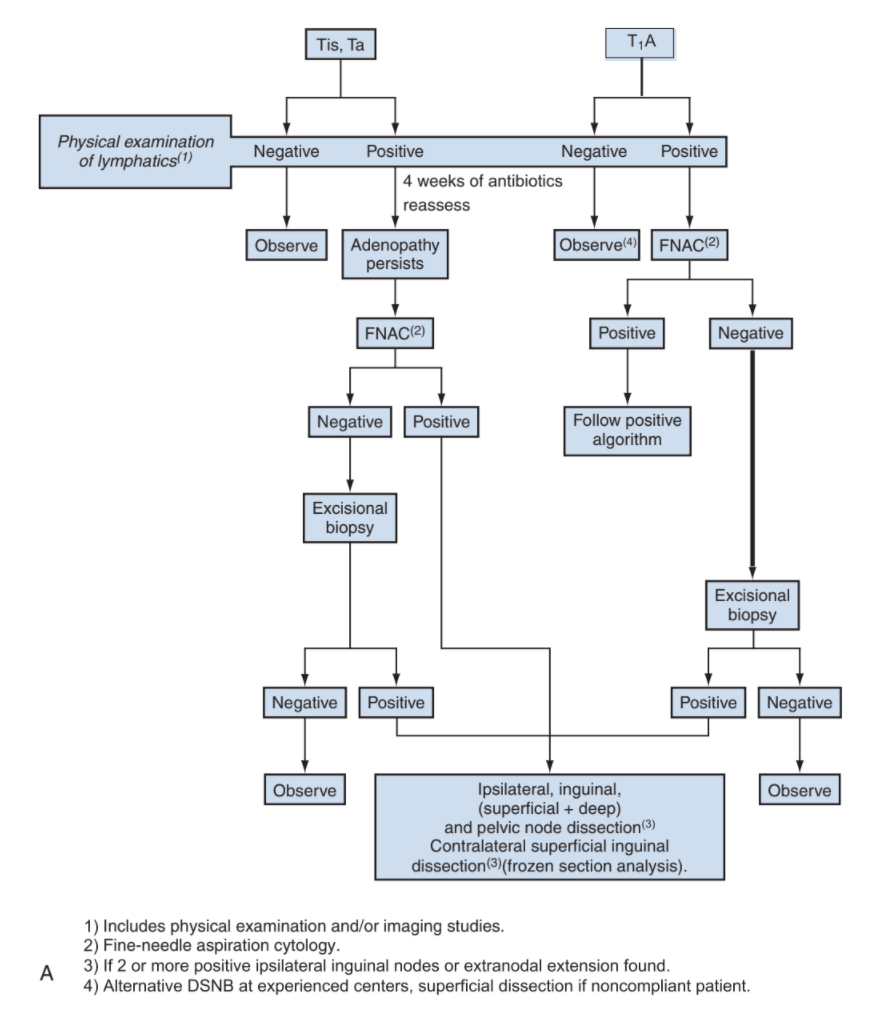
Nodal Management
Evaluation
- Indications for intervention: any primary tumor besides Tis, Ta, or T1 (with low grade) - 0-16% +LN rate
- Nonpalpable nodes: 1/4 have ILN metastases, therefore ILND recommended if risk factors present despite nonpalpable nodes
- Palpable nodes: consider needle biopsy (93% sensitivity and 91% specificity),avoids giving patients 4-6 weeks antibiotics prior to considering surgery
- Dynamic Sentinel Node Biopsy (DSNB): inject Tc99 + blue dye at tumor/scar site 1 day prior, then excise sentinel node, < 15% false negative rate in experienced centers (> 20/yr), offer for non-palpable nodes only
Inguinal Node Anatomy
- Superficial inguinal node boundaries: external oblique fascia superiorly, sagittal plane through ASIS laterally, sagittal plane through pubic tubercle medially, transverse plane 20cm inferior to ASIS inferiorly
- Deep inguinal nodes: found within femoral triangle (sartorius, inguinal ligament, adductor longus), covered by fascia lata, avoid dissection lateral to femoral artery
- Node of Cloquet: most cephalad deep ILN
- Radical ILND: uses full superficial boundaries, requires saphenous vein ligation at junction with femoral vein, place sartorius muscle flap
- Modified ILND: avoid removal of nodes inferior to fossa ovalis and lateral to femoral artery, can still perform deep dissection
ILND tips
- Modified vs Radical template: use modified for non-palpable nodes, convert to radical if cancer present, higher false-negative rate with modified (5.5% vs 0%)
- Bilateral ILND unilateral adenopathy, due to presence of bilateral drainage - may not be indicated if delayed adenopathy after primary treatment
- Make incision transverse to minimize risk for skin necrosis
- Early mobilization: recommended unless flap used (bedrest 48-72hr)
- Postoperative antibiotics: x1 week or until drains removed
- Drain duration: continue until < 100-150mL/d
- Complications: wound issues (0.6-43%), lymphedema + lymphocele + seroma (2.4-26.5%)
- Delaying ILND by > 12 weeks decreases 5yr survival 64% to 40%
- Pelvic LND consider if 2+ LN in ILND, mets in node of Cloquet, extra-nodal extension, or imaging concerning for pelvic mets
Prognosis
- Predictors of long-term survival: ≤ 2 LNs +, unilateral disease, no ENE, and no pelvic metastases
- 5yr survival: 90-100% for negative ILND, 80% for 1 positive node, 50% for 2+ unilateral nodes, and 10% for bilateral positive nodes, extranodal extension, or positive pelvic nodes
References
- AUA Core Curriculum
- Kutikov, A., P. L. Crispen, and R. G. Uzzo. "Pathophysiology, evaluation, and medical management of adrenal disorders." Campbell-Walsh Urology 12 (2020).
- Pettaway, C., J. Crook, and L. Pagliaro. "Tumors of the Penis." Campbell-Walsh Urology 12 (2020).
- Sotelo, R., L. Medina, and M. Machado. "Inguinal Node Dissection." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.