Bladder Cancer Evaluation
Bladder Cancer Presentation
Bladder Cancer Risk Factors
- Tobacco use: increases risk by 2-3x
- Chemical exposure: aromatic amines, polycyclic aromatic hydrocarbons, arsenic
- Cyclophosphamide: used for lymphoma and leukemia, risk is dose dependent, 4.5x increased risk, unclear if mesna reduces risk for bladder cancer (does reduce hemorrhagic cystitis risk)
- Lynch Syndrome: UTUC risk higher than bladder cancer
- Other syndromes: Peutz-Jegher, Cowden, Li-Fraumeni, Costello, NF1
- Schistosomiasis: endemic in 76 countries, causes SCC
- History of pelvic XRT: 15-30yr latency period, 2-4x higher for cervical cancer patients, EBRT more likely cause than brachytherapy for prostate cancer
- Chronic catheter use: increased risk of SCC from chronic inflammation, surveillance not warranted
- Pioglitazone: has been shown to have an increased risk (PROactive trial), increases absolute risk by 0.03%
- Arsenic: causes Blackfoot disease (seen in Taiwan), with hyperkeratosis and cardiac issues
- Non-risk factors: fluid intake, food, caffeine, alcohol
Presentation
- Microscopic hematuria: seen in almost 100% bladder cancer patients at presentation - 2.6% AMH workups are diagnosed malignancy
- Gross hematuria: seen in 85% bladder cancer patients at presentation - 20% gross hematuria patients are diagnosed with malignancy
- Dysuria without UTI: suspect carcinoma in situ
- Mass on CT/MR: can skip cystoscopy, go straight to TURBT
- Red patch (Swinn 2004): 12% positive cancer rate, majority are CiS, more likely malignant if > 60yo
- Cytology: not useful for screening, but worth checking if history of HG or CiS disease - 60-70% sensitivity, vs only 10-30% for LG disease
- Cytology for equivocal lesions: Svatek 2005 reported in patients with no bladder cancer history, positive cytology was 100% sensitive and had 100% NPV for equivocal lesions, whereas any truly concerning lesion (papillary/sessile) was almost always cancer
- Hydronephrosis: concerning (but not diagnostic) for muscle-invasive disease
- Upper tract imaging (CTU/MRU): obtain prior to TURBT if able, rules out hydronephrosis or upper tract disease - accuracy 72% for perivesical invasion, 86% for LN metastasis
Obtain Diagnosis with TURBT
TURBT Tips
- Blue light: HAL preferentially accumulates in tumors, detects 15% more Ta and 41% more CiS, decreases recurrence rates, wait 3mo after BCG (increased false positive rates)
- Narrow band: enhances contrast between surfaces, decreases recurrence rates (27%->6%)
- CiS management: if widespread then avoid fulgurating entire bladder, consider biopsies of prostate and adjacent to papillary lesions
- Obturator reflex prevention: avoid overdistension, decrease current, obturator nerve block, general anesthesia + paralysis
- Cytology: more sensitive for HG/CiS (positive in 54-57%), less sensitive for LG
- Clinic fulguration: can perform for suspected TaLG lesions
- Stenting: not required when ureteral orifice is resected, but use cutting current only with quick strokes, 4% postop hydronephrosis (check in 3-6wk with imaging), potentially increases upper tract risk x3-4 (no difference in risk between stent and PCN)
- Use 70 degree lens to evaluate bladder neck
- Negative cystoscopy + positive cytology: random bladder biopsy -> prostatic biopsy -> retrograde pyelograms +/- upper tract cytology -> diagnostic ureteroscopy
- Random bladder biopsy indications: considering partial cystectomy, no visible bladder tumors but positive cytology (see above), HG cytology but LG path, after CiS intravesical therapy
- Prostatic urethral biopsy indications: multifocal disease, bladder neck tumors, CiS, abnormal urethral appearance, positive cytology without source (see above)
- True perforations: rare (0.36%), intraperitoneal require exploration + closure
- TURP at time of TURBT: no proven risk of prostatic urethral seeding
Post-TURBT intravesical chemotherapy
- Indications: presumed low/intermediate risk (usually Ta disease)
- Efficacy: reduces risk of recurrence by 10-15% (NNT=7.2)
- Timing: within 6hrs (24hr okay but less ideal) after TURBT, hold in bladder for 60 minutes
- Contraindications: concern for perforation or extensive resection
Repeat TURBT
- Timing: 4-6wks after initial TURBT
- Indications: all T1 disease (even if muscle present), high risk Ta disease (if no muscle or incomplete resection), incomplete resection (R1), or variant histology (if attempting to avoid cystectomy)
- Overall: 40% have residual disease on repeat TURBT
- High risk Ta disease: residual tumor present in up to 50% TaHG, 15% get upstaged
- T1 disease: 15-20% upstaged if muscle present vs 40-50% upstaged if muscle not present on initial TURBT
- Residual T1 on reTURBT: up to 80% risk of progression to MIBC
UTUC Workup
- < 2-5% patients with bladder cancer have UTUC
- Upper tract imaging is recommended (by AUA guidelines) at first diagnosis of bladder cancer
- Risk factors: CiS, high grade NMIBC, trigonal tumors
- 0.8-10% will eventually develop UTUC
Bladder pathologies
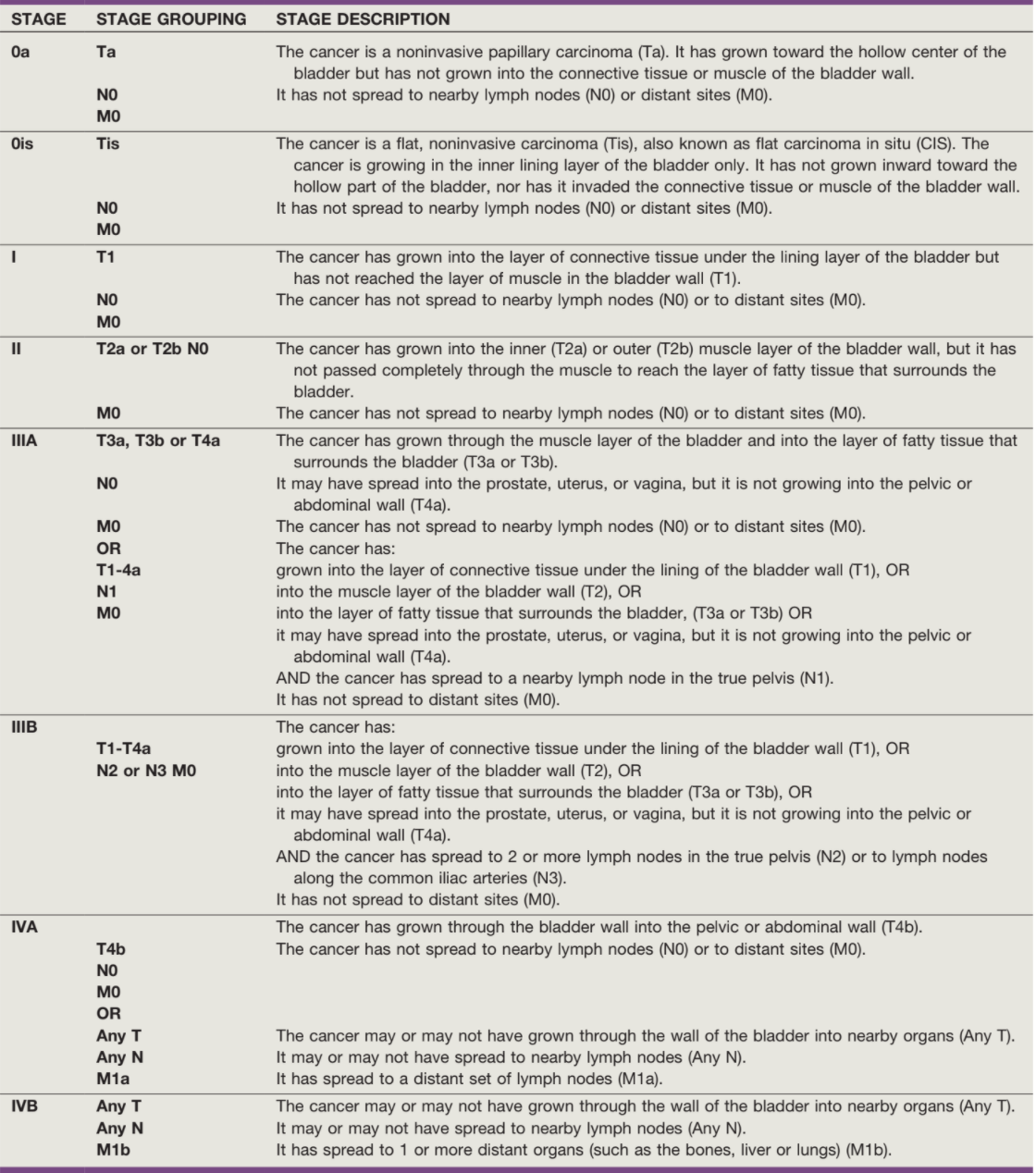
NMIBC vs MIBC
- NMIBC (70-80%): Ta (noninvasive, 60-70%), T1 (lamina propria (20-30%)), TiS (10%)
- MIBC (20-30%): T2 (muscularis propria), T3 (perivesical fat), T4a (prostate, vagina), T4b (pelvic sidewall)
Non-malignant TURBT findings
- Squamous metaplasia: seen in 40% women and 5% men, no biopsy/treatment required
- Inverted papilloma: benign, can cause hematuria, 1% chance recurrence, grow in endophytic pattern with nests in lamina propria
- Papilloma: benign, stalks with normal urothelium
- Leukoplakia: similar to squamous metaplasia but shows flaky plaques floating in the bladder, presents with rUTI + frequency + urgency, no longer considered pre-malignant
- Cystitis cystica and follicular cystitis: common, seen with chronic inflammation/obstruction and recurrent UTIs, no malignancy risk
- Eosinophilic cystitis: allergic reaction, biopsy shows eosinophils in urothelium, manage with anticholinergics, antihistamines, and steroids
- Granulomatous cystitis: seen with TB infection and BCG therapy, manage with isoniazid + B6 (if BCG) or RIPE (if TB)
- Malakoplakia: brownish bladder plaques, histology shows von Hansemann cells (granular macrophages) with Michaelis-Gutmann bodies (targetoid inclusions), treat with resection and antibiotics
- Amyloidosis: appears like cancer, confirm diagnosis and workup with amyloid expert, manage with TURBT and intravesical DMSO
Premalignant and recurrent TURBT findings
- Cystitis glandularis: potential malignant transformation (adenocarcinoma), regular surveillance
- Inflammatory myofibroblastic tumor: appears as a tumor, spindle cells with inflammation, manage with TURBT, regular surveillance
- Nephrogenic adenoma: caused by chronic irritation, present with hematuria/dysuria, treated with resection, can recur
- Bladder leiomyoma: arise from detrusor, seen as smooth bulge under urothelium, require TURBT or partial cystectomy
- Bladder paraganglioma: present with hematuria/HTN, can cause hypertensive crisis during TURBT, treat with resection
- Hemangioma: can cause hematuria, usually seen in patients < 30yo, manage with resection, can be seen in Sturge-Weber syndrome
Variant Histology
- Micropapillary: 0.7-2.2% prevalence, 50+% are T3-T4, 51% and 24% 5 and 10 year survival, does not respond to BCG or NAC
- Sarcomatoid: 0.3-0.6% prevalence, 28% 5yr cancer-specific survival
- Plasmacytoid: < 1% prevalence, responds to NAC but commonly relapses, risk for causing peritoneal carcinomatosis
- Nested: rare, often locally invasive
- Squamous differentiation: 16-22% prevalence, higher risk of progression/recurrence
- Glandular differentiation: 10% prevalence, similar recurrence rates
- Management: poor response to intravesical chemotherapy, variants (with mainly urothelial) have similar response to neoadjuvant chemotherapy (per Hajiran 2021) vs worse outcomes for differentiation histology, consider up-front cystectomy or repeat TURBT (if attempting bladder sparing approach)
- Stage: 64% are found to have T3-T4 disease during cytectomy as opposed to only 34% for pure urothelial histology
Non-Urothelial Bladder Cancers
- Small cell: aggressive but chemosensitive, treated with platinum based therapies, 78% 5yr survival with cisplatin/etoposide then cystectomy vs 36% for up front cystectomy (possibly due to higher stage at presentation), if metastatic treat with chemotherapy alone
- Squamous cell: no benefit to NAC, managed with up front cystectomy (+/- urethrectomy), can consider XRT
- Adenocarcinoma: may be due to direct extension or metastatic disease (most common cause), should undergo screening colonoscopy/endoscopy, check CEA, check PSA in men, check Ca-125 and mammogram in women, treat primary with up front cystectomy (minimal benefit with chemo/XRT), if metastatic treat primary disease
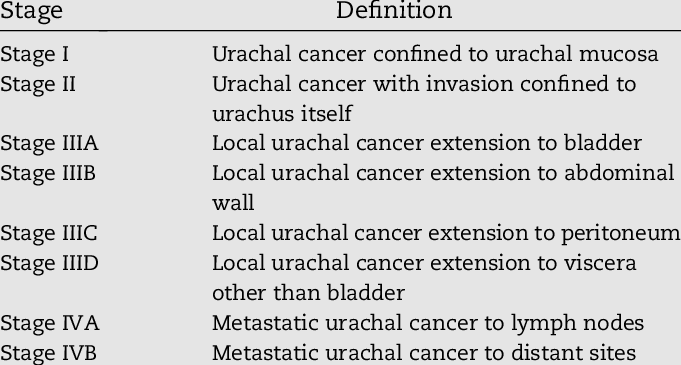
- Urachal cancer: rare, check CEA, treat with en bloc resection of bladder dome + urachal ligament + umbilicus
References
- AUA Core Curriculum
- Anderson, C. and J. McKiernan. "Tumors of the Urethra." Campbell-Walsh Urology 12 (2020).
- Chang, Sam S., et al. "Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline." The Journal of urology 196.4 (2016): 1021-1029.
- Chang, Sam S., et al. "Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline." The Journal of urology 198.3 (2017): 552-559.
- Djaladat, Hooman, et al. "Reproductive organ involvement in female patients undergoing radical cystectomy for urothelial bladder cancer." The Journal of urology 188.6 (2012): 2134-2138.
- El-Achkar, Adnan, Luis Souhami, and Wassim Kassouf. "Bladder preservation therapy: review of literature and future directions of trimodal therapy." Current urology reports 19.12 (2018): 1-10.
- Grossman, H. Barton, et al. "Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer." New England Journal of Medicine 349.9 (2003): 859-866.
- Guzzo, T., J. Christodouleas, and D. Vaughn. "Management of Muscle-Invasive and Metastatic Bladder Cancer." Campbell-Walsh Urology 12 (2020).
- Hajiran, Ali, et al. "Pathological and survival outcomes associated with variant histology bladder cancers managed by cystectomy with or without neoadjuvant chemotherapy." The Journal of urology 205.1 (2021): 100-108.
- Jarret, T., S. Matin, and A. Smith. "Surgical Management of Upper Urinary Tract Urothelial Tumors." Campbell-Walsh Urology 12 (2020).
- Kallidonis, P., and E. Liatsikos. "Urothelial Tumors of the Upper Urinary Tract and Ureter." Campbell-Walsh Urology 12 (2020).
- Kates, M., and T. Bivalacqua. "Tumors of the Bladder." Campbell-Walsh Urology 12 (2020).
- Lamm, Donald L., et al. "Maintenance bacillus Calmette-Guerin immunotherapy for recurrent TA, T1 and carcinoma in situ transitional cell carcinoma of the bladder: a randomized Southwest Oncology Group Study." The Journal of urology 163.4 (2000): 1124-1129.
- Margulis, Vitaly, et al. "Preoperative multivariable prognostic model for prediction of nonorgan confined urothelial carcinoma of the upper urinary tract." The Journal of urology 184.2 (2010): 453-458.
- Navai, N. and C. Dinney. "Surgical Management of Bladder Cancer: Transurethral, Open, and Robotic." Campbell-Walsh Urology 12 (2020).
- Sheldon, Curtis A., et al. "Malignant urachal lesions." The Journal of urology 131.1 (1984): 1-8.
- Sountoulides, Petros, et al. "Does ureteral stenting increase the risk of metachronous upper tract urothelial carcinoma in patients with bladder tumors? A systematic review and meta-analysis." The Journal of Urology 205.4 (2021): 956-966.
- Svatek, Robert S., David Lee, and Yair Lotan. "Correlation of office-based cystoscopy and cytology with histologic diagnosis: how good is the reference standard?." Urology 66.1 (2005): 65-68.
- Swinn, M. J., et al. "Biopsy of the red patch at cystoscopy: is it worthwhile?." European urology 45.4 (2004): 471-474.
- Sylvester, Richard J., et al. "Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials." European urology 49.3 (2006): 466-477.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.
- Woldu, Solomon L., Aditya Bagrodia, and Yair Lotan. "Guideline of guidelines: non‐muscle‐invasive bladder cancer." BJU international 119.3 (2017): 371-380.
- Zabell, J., and B. Konety. "Management Strategies for Non-Muscle-Invasive Bladder Cancer." Campbell-Walsh Urology 12 (2020).