Benign and Malignant Adrenal Masses
Benign Adrenal Neoplasms
Adrenal Adenomas
- Prevalence: 0.5% if in 20s, 7% if 70+yo, 6% of autopsy patients
- 85-90% incidentally diagnosed adrenal masses are adenomas, with 7% of these exhibiting hormone secretion
- Subsequent function: 1.7% nonfunctional adenomas gained function on follow-up
- The goal of the workup is to rule out malignancy and metabolic/hormonal activity
- CT imaging: < 10HU on noncontrast CT and > 40-60% contrast washout are highly likely to be adenomas
- Need for follow-up after workup is controversial due to low rates of growth and hormonal activity
Other adrenal lesions (all are rare)
- Oncocytoma: > 30% reported as malignant, surgery recommended
- Myelolipoma: can rupture (more common if > 10cm), diagnosed based on CT appearance, observe unless symptomatic
- Ganglioneuroma: CT may show < 40HU and stippled calcifications
- Cysts: CT imaging w/ sharply marginated fluid without enhancement, cyst excision/aspiration may be required to rule out malignancy, most can be observed
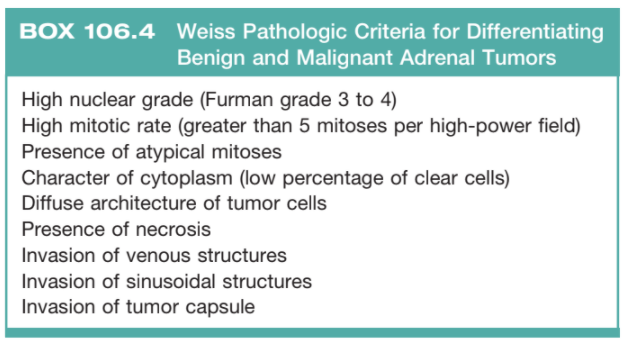
Weiss Criteria, from Campbell's
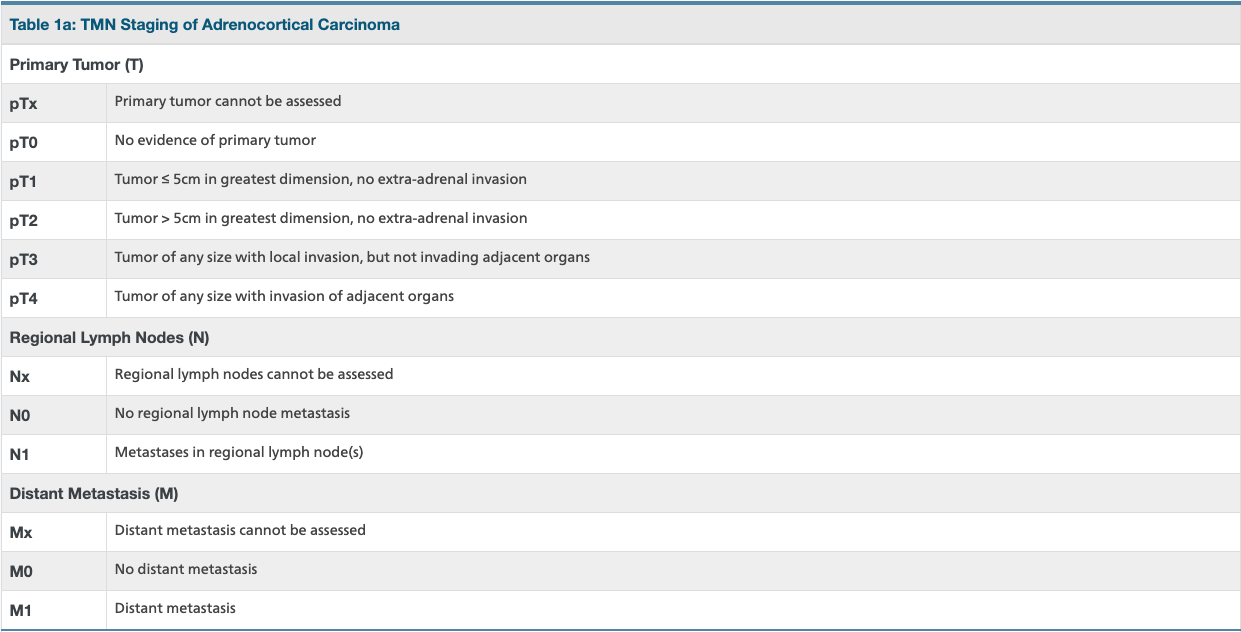
Adrenocortical carcinoma TNM staging, from AJCC
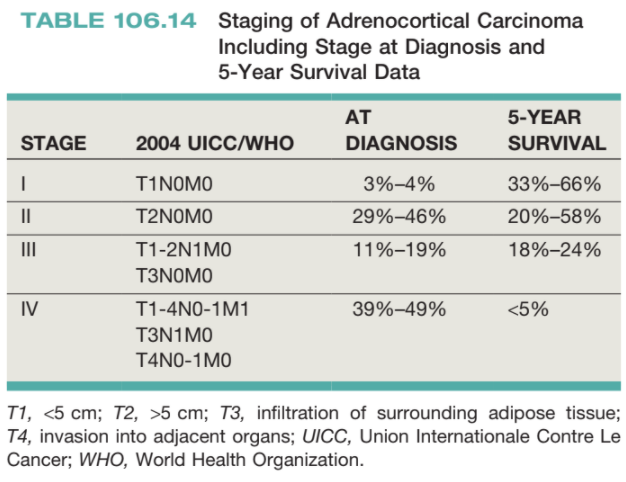
5yr survival of ACC, from Campbell's
Adrenal Malignancies
Primary Adrenocortical Carcinoma (ACC)
- Common symptoms: hormonal hypersecretion (40-60%), abdominal pain/fullness (30%)
- Test for steroid hormones as well as precursor molecules
- Imaging: CT/MR A/P, larger tumors more likely to be malignant (10% if > 4cm, 25% if > 6cm), usually > 25HU on non-contrast imaging and < 50% washout, chest imaging is required, bone scan and MR head only if bone/neuro symptoms
- Weiss criteria: 3+ criteria have 100% sensitivity and 96% specificity for diagnosing malignant vs benign adrenal masses
- Surgical resection recommended, with en bloc resection
- Consider removal of mass and metastases if able to remove > 90% disease burden
- Surveillance: CT C/A/P q3mo for 2-3yrs, then space out to q6mo until 5yrs postop
- XRT: recommended for CNS and bone metastases
- Mitotane: DDT derivative, most commonly used adjuvant chemotherapy
- Overall 5yr survival 20-47%
Metastases to the Adrenal Gland
- Prevalence: in setting of prior extra-adrenal malignancy, > 50% newly diagnosed adrenal lesions are metastatic disease
- Imaging: metastases tend to be lipid-poor, > 10HU on noncontrast CT and do not show contrast washout, risk of malignancy is 7% if otherwise benign-appearing on CT
- Treatment: can consider biopsy, adrenalectomy, or surveillance depending on clinical scenario
- Adrenalectomy: recommended for RCC if radiographically abnormal or tumor thrombus in the renal vein
- Surveillance: screen adrenal mass at same interval as primary malignancy
- Biopsy: only if not metabolically active, not clearly benign on imaging, and pathology results would alter management
References
- AUA Core Curriculum
- Fassnacht, Martin, et al. "Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European network for the study of adrenal tumors." European journal of endocrinology 175.2 (2016): G1-G34.
- Lim, SK. and K. Ho Rha. "Surgery of the Adrenal Glands." Campbell-Walsh Urology 12 (2020).
- Maas, Marissa, et al. "Discrepancies in the recommended management of adrenal incidentalomas by various guidelines." The Journal of Urology 205.1 (2021): 52-59.
- Kutikov, A., P. L. Crispen, and R. G. Uzzo. "Pathophysiology, evaluation, and medical management of adrenal disorders." Campbell-Walsh Urology 12 (2020).