Overactive Bladder Workup
Definitions
- OAB: urgency +/- frequency, nocturia, and urge incontinence
- Urgency: sudden compelling desire to pass urine that is difficult to defer
- Frequency: > 7 voids during the day
- Nocturia: 1+ nocturnal voids
- Nocturnal polyuria: large production of urine during sleep, > 20% if younger, > 33% if older
- Polydipsia: normal/large volume voids (OAB causes small volume voids)
- Urge incontinence: involuntary urine leakage associated with sudden desire to void
- Interstial Cystitis: may have frequency/urgency, but pain is prime symptom (no pain in OAB)
- Complicated OAB: failure to respond to medications, young age, hematuria, rUTI, pelvic prolapse, fecal incontinence, constipation, hx GU cancer, hx GU surgery, hx pelvic XRT, hx neurologic disease, impaired mobility, poor DM control
History
- Storage symptoms: frequency, urgency, urge incontinence, nocturia
- Voiding symptoms: hesitancy, straining, retention, stream strength, intermittency
- Fluid intake habits: types, volume, void diary
- Degree of bother
- PMHx: neuro diseases, mobility issues, DM, BM habits, pelvic pain, rUTIs, hematuria, pelvic cancers, pelvic XRT, prolapse
- PSHx: pelvic surgery, pregnancies
- Bowel habits: constipation, diarrhea, fecal incontinence (seen in up to 50% with OAB)
- Meds: diuretics
Physical
- Abdominal exam: scars, masses, hernias, SP distension
- Lower extremities: edema - fluid overload
- Pelvic exam: atrophic vaginitis, prolapse, stress incontinence, pelvic floor dysfunction, BPH
- Cognitive function and frailty
Adjuncts
- Symptom questionnaires: UDI, UDI-6, II-Q, OAB-q
- Urinalysis: always obtain, consider separate workup if evidence of hematuria or UTI
- PVR and urine culture: not required for uncomplicated patients
- Other testing: CT/US, urodynamics, cystoscopy, and cytology are not required for uncomplicated patients
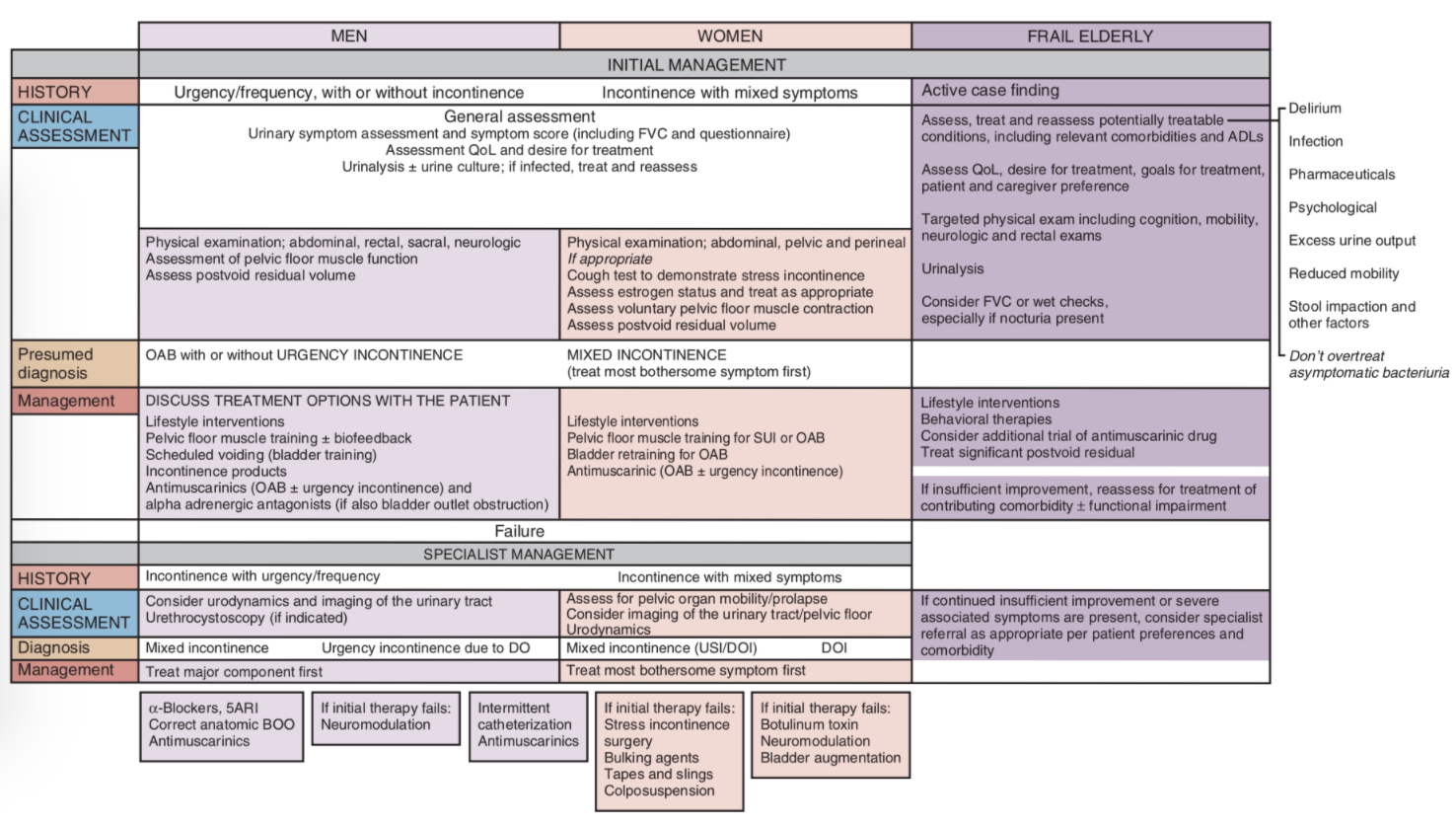
Considerations for men
- Cause: often secondary to BPH/BOO, resulting in detrusor overactivity
- Incontinence: much less prevalent (16% vs 55%)
- Retention risk: < 3% with anticholinergics, but not recommended if flow rate < 5mL/s or PVR > 200mL
- Post-outlet treatment: OAB resolution seen in 70%, can take up to 6-12mo to improve (keep on medications until this time)
References
- AUA Core Curriculum
- Gormley, E. Ann, et al. "Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline." The Journal of urology 188.6S (2012): 2455-2463.
- Heesakkers, J. and B. Blok. "Electrical Stimulation and Neuromodulation in Storage and Emptying Failure." Campbell-Walsh Urology 12 (2020).
- Herschorn, Sender, et al. "Efficacy and safety of combinations of mirabegron and solifenacin compared with monotherapy and placebo in patients with overactive bladder (SYNERGY study)." BJU international 120.4 (2017): 562-575.
- Reynolds, W. and J. Cohn. "Overactive Bladder." Campbell-Walsh Urology 12 (2020).