Urodynamic Terminology and Normal Findings
Urodynamic Terminology
The Many Cs of Urodynamics
- Capacity: volume
- Compliance: DLPP
- Contractility: DO, DUA
- Coordination: DESD
- Continence: VLPP
- Conscious sensation: increased/decreased
- Complete emptying: DUA, BOO
- Clinical obstruction: BOO
Broad classifications for voiding dysfunction
- Storage dysfunction vs emptying dysfunction
- Bladder dysfunction vs bladder outlet dysfunction
Urodynamic components
- Cystometry: pressure/volume relationship of the bladder during filling, measures sensation, compliance, capacity, and presence of detrusor activity
- Electromyography (EMG): measurement of sphincter (and pelvic) muscle depolarization
- Pressure-flow studies: bladder pressure and urine flow rate during emptying
- Uroflowmetry: measurement of urine flow rate
- Video UDS: fluoroscopy during UDS
Normal urodynamics
Measurements
- Compliance: change in volume over change in pressure, < 6cm water increase considered normal
- Cough leak point pressure (CLPP): urinary leakage with cough, considered superior to VLPP
- Detrusor leak point pressure (DLPP): detrusor pressure at which urine leakage occurs in the absence of detrusor contraction or increased abdominal pressure, 40cm water usually used as cutoff for concern for renal injury
- Maximum urethral closure pressure (MUCP): max difference between urethral and intravesical pressures
- Post Void Residual: amount of urine left in bladder after urination, no universal definition, elevated PVR caused by DUA and/or BOO
- Urethral pressure profile: fluid pressure needed to open a closed urethra
- Valsalva leak point pressure (VLPP): intravesical pressure at which urine leakage occurs in the absence of a detrusor contraction, tends to be lower than CLPP
- Volumes: first sensation, sensation of fullness, desire to void, capacity
Filling phase
- Detrusor pressure should remain near zero until voiding is initiated
- Detrusor pressure (Pdet): differentiate between Valsalva (Pdet unchanged) and true detrusor contraction (Pdet rises)
- Impaired compliance: > 40, needs treatment to prevent upper tract injury, may be artificially decreased if reflux or diverticulum present
- Abdominal leak point pressure (ALPP): ability of sphincter to resist changes in abdominal pressure, can only be seen with SUI, < 60 indicates ISD, > 90 indicates minimal/no ISD
- Stress induced detrusor overactivity (SIDO): triggered by rise in abdominal pressure
Emptying phase
- Normal voiding: relaxation of striated sphincter, detrusor contraction, opening of bladder neck and urethra, onset of urination
- Minimum volume 150mL recommended to assess uroflow curve
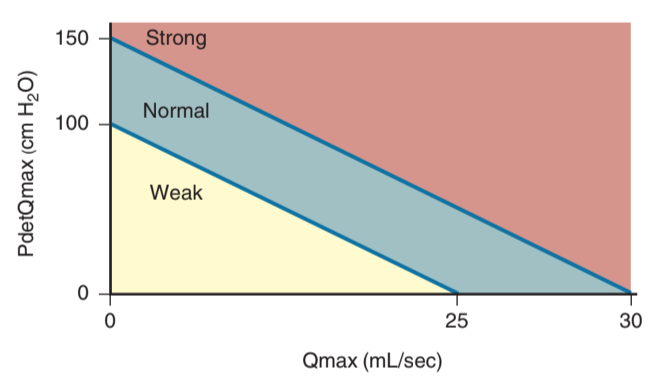
- Detrusor underactivity (DUA): low pressure and low flow, reduced contraction strength leading to prolonged emptying time
- Detrusor acontractility: no detrusor contraction on UDS
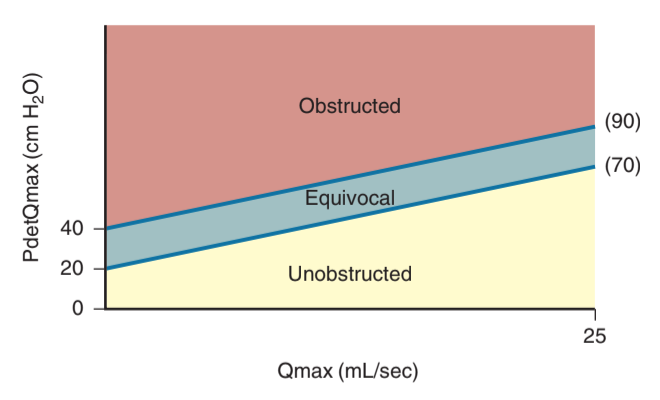
- Bladder outlet obstruction: high pressure and low flow
- Abrams Griffiths nomogram: BOOI = PdetQmax - 2 * Qmax
- Bladder contractility index (BCI, Schafer's lines): PdetQmax + 5 * Qmax
VideoUDS
- Indications: localize level of obstruction, detect incontinence, evaluate for reflux
- Findings: bladder contour, trabeculations, diverticula, stones, reflux, bladder neck, urethra
- The only method available for diagnosing primary bladder neck obstruction
References
- AUA Core Curriculum
- Brucker, B. and V. Nitti. "Urodynamic and Video-Urodynamic Evaluation of the Lower Urinary Tract." Campbell-Walsh Urology 12 (2020).
- Reynolds, W. and J. Cohn. "Overactive Bladder." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.
- Winters, J. Christian, et al. "Urodynamic studies in adults: AUA/SUFU guideline." The Journal of urology 188.6 (2012): 2464-2472.