Nocturia
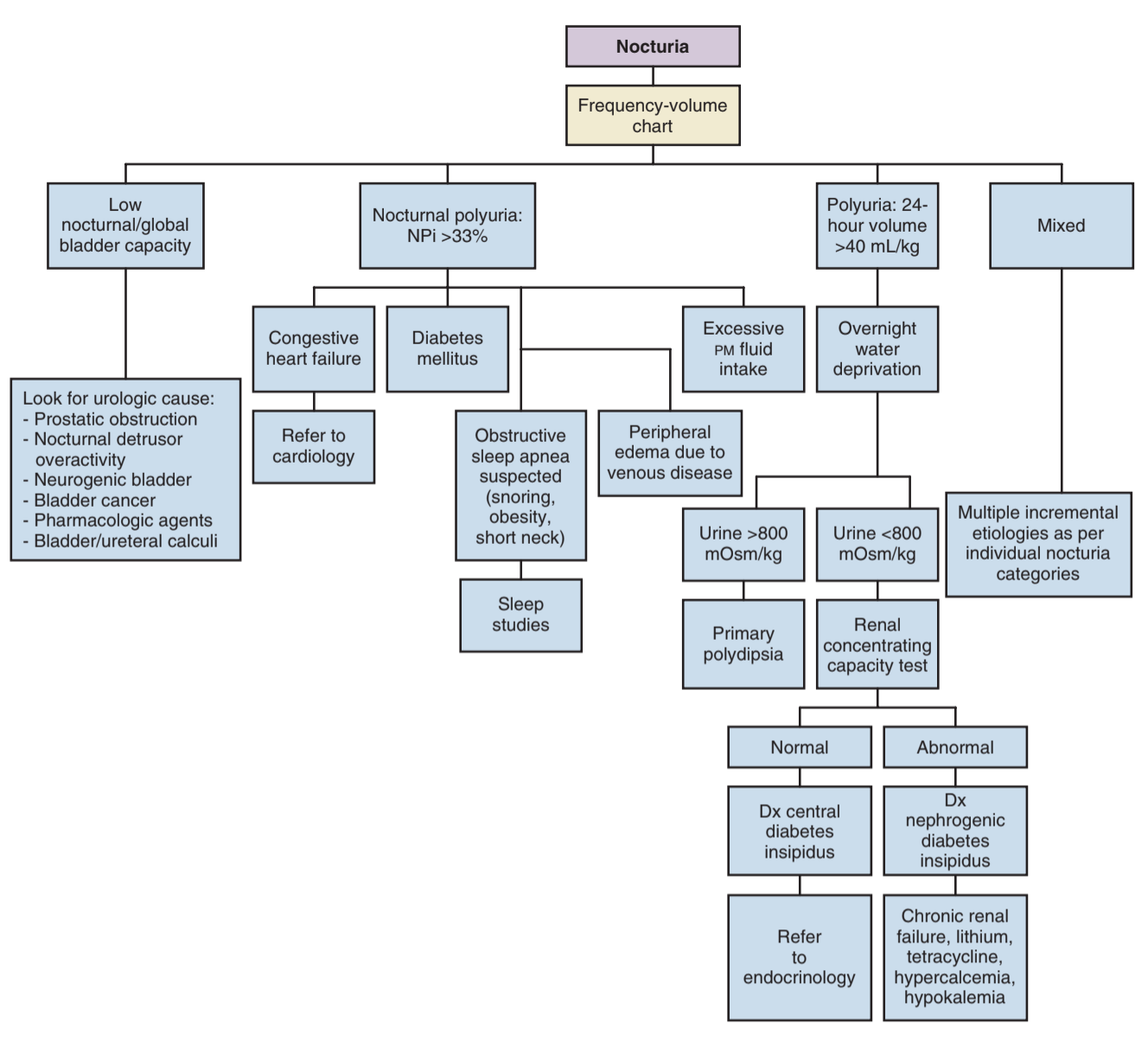
Evaluation
Initial workup
- Evaluation: fluid intake, other LUTS, sleep habits, medications (pre-bedtime), OSA symptoms, medical conditions (cardiac, DM), prior pelvic surgeries, dysuria
- Sleep apnea: multiple mechanisms lead to decreased ADH secretion and poor sleep hygiene, screen with STOP BANG questionnaire, treating underlying OSA often improves nocturia symptoms, nocturia may be just as predictive as snoring for OSA
- Medications: diuretics (if taken too close to bedtime), antidiuretics (if taken too early in AM), edema-inducers, CNS modifiers, or bladder irritants
Calculations
- Nocturia index (Ni): total nocturnal urine volume (including first morning void) divided by maximum voided volume, if > 1 then either nocturia or enuresis occurs
- Nocturnal bladder capacity index (NBCi): # nocturnal voids (not including first morning void) minus Ni-1, if > 0 then nocturia is related to decreased bladder volumes
- Nocturnal polyuria index (NPi): nocturnal urine volume divided by 24hr total volume, normal NPi 0.20 if 21-65yo vs 0.34 for > 65yo, other definitions include NUV > 90mL/hr, > 6.4mL/kg, > 0.9mL/min
Management
Conservative management
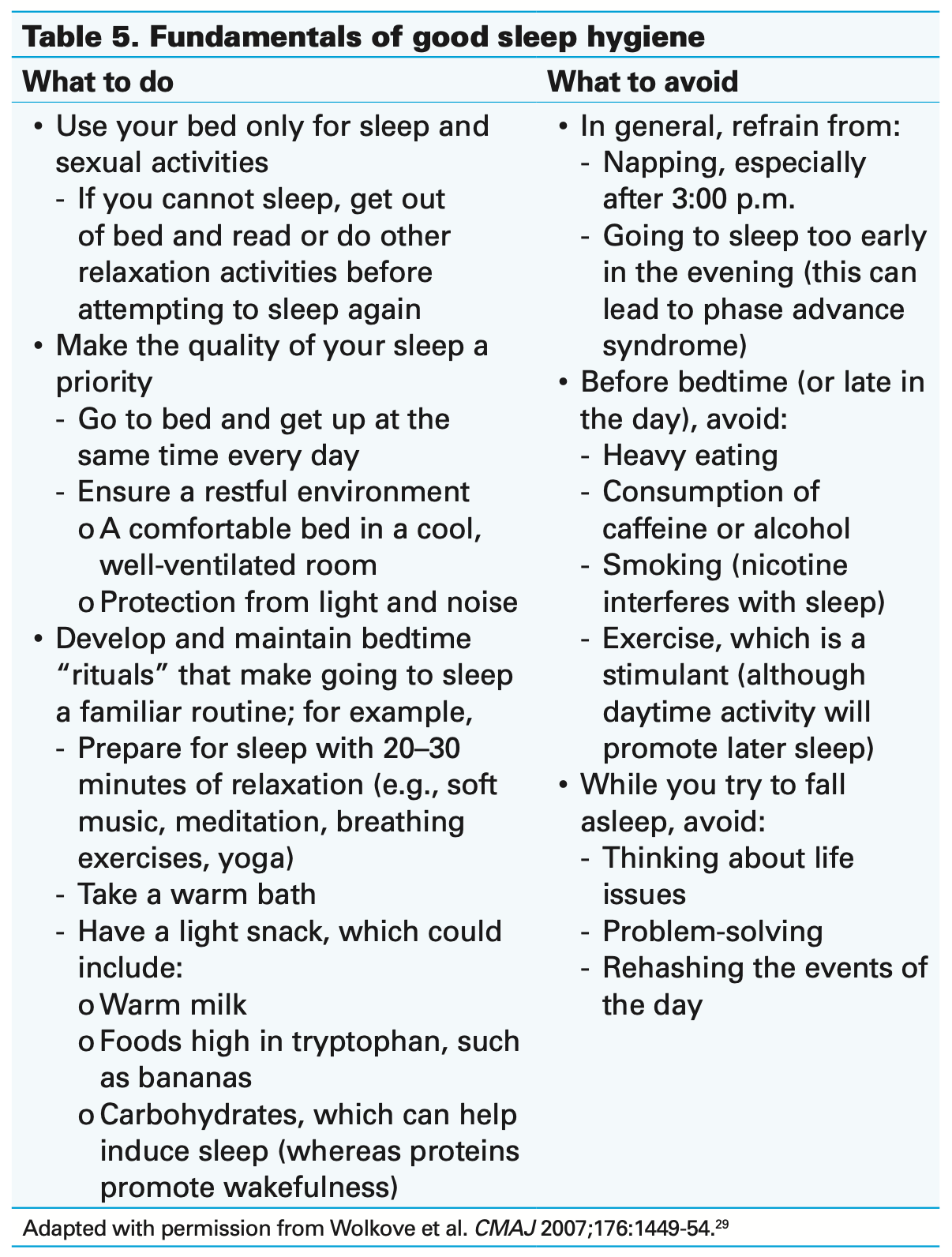
- Fluid restrictions: minimize fluids 2-4hr before bed, minimize alcohol/caffeine
- Dietary changes: salt can increase fluid retention, evening protein can increase urea (and therefore urine) output
- Obesity: diet changes can improve salt/protein intake, worsens OSA risk, exercise can improve sleep hygiene
Specific recommendations
- Peripheral edema: elevate legs above heart level 1-3hr before bed, compression stockings, diuretic use (20mg furosemide 6-8hr before bed)
- Bladder outlet obstruction: benefit especially if elevated post-void residual, nocturia improves in 18% with tamsulosin and 32% after TURP (decreases average 1.3 voids/night)
- Reduced bladder capacity: may benefit from physical therapy and bladder training to improve bladder volumes, very frequent nocturia secondary to severe urgency respond best to medical management
- Sleep apnea: patients benefit from sleep evaluation to rule out as underlying cause, encourage CPAP use
Desmopressin
- Indications: nocturnal polyuria
- Dosing: 50-200ug PO (or 60-240ug sublingual) 1hr before bed
- Contraindications: severe liver disease, heart failure, and renal failure (GFR < 50)
- Side effects: nausea, diarrhea, dizziness, hypertension, hyponatremia
- Hyponatremia risk factors: > 65yo, renal dysfunction, low BMI, female, baseline low-normal sodium levels
- Monitoring: check for hyponatremia at 7 days, 28 days, and q6mo
Global polyuria
- Definition: 24hr UOP > 40mL/kg
- Causes: diabetes mellitus, diabetes insipidus, primary polydipsia
- Overnight water deprivation test (OWDT): restrict fluid intake for 8hr, give 2ug IM desmopressin, then check urine osmolality, differentiates primary polydipsia (> 800mOsm/kg) vs diabetes (< 800mOsm/kg)
- Diabetes differential: check glucose and HbA1c to differentiate mellitus from insipidus
- Renal concentrating capacity test (RCCT): differentiates central (uOsm > 800) vs nephrogenic (uOsm < 800) diabetes insipidus, 40ug intranasal or 0.4mg PO desmopressin and empty bladder, measure uOsm 3-5hrs later
References
- AUA Core Curriculum
- Marshall, S. and J. Weiss. "Nocturia." Campbell-Walsh Urology 12 (2020).
- Nguyen, Laura N., et al. "Canadian Urological Association best practice report: Diagnosis and management of nocturia." Canadian Urological Association Journal 16.7 (2022): E336.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.