Neuromuscular Lower Urinary Tract Dysfunction Evaluation
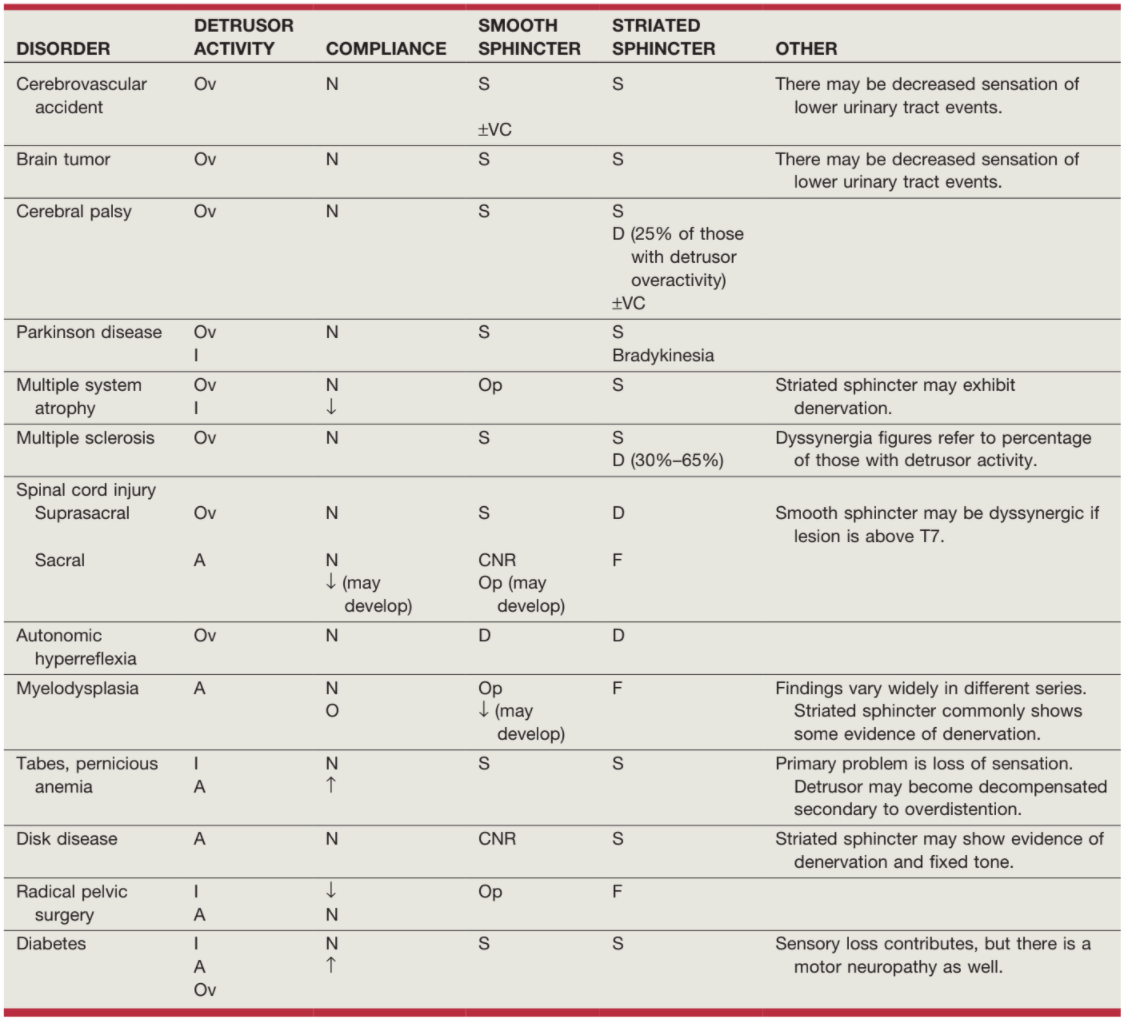
Common patterns of voiding dysfunction, from Campbell's
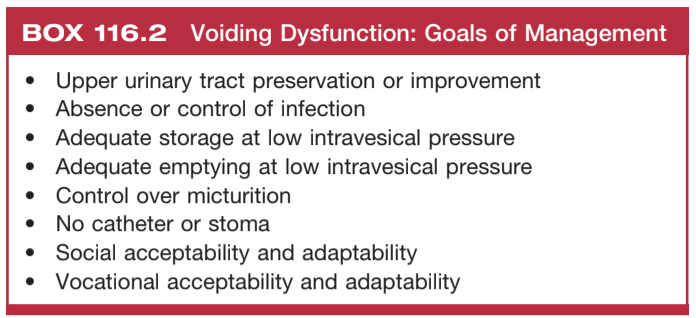
Goals for managing LUT dysfunction, from Campbell's
Initial Evaluation
Evaluation
- Urinalysis: not required for regular screening, pyuria and hematuria normal/expected with catheterization
- Cystoscopy: warranted for rUTI, hematuria, or anatomic abnormalities, but screening surveillance not warranted even if chronic catheter (no benefit to bladder cancer cystoscopy screening), consider screening bladder augments
- Renal function: trend creatinine, may be abnormally low compared to non-NMLUTDS, alternatives include Cystatin C and renal scan
- Urodynamics timing: do not perform in acute setting of spinal shock or brain injury, as symptoms and neural pathways may change as injury heals over 6-24mo
- Probability of regaining volitional voiding at 1yr (per ASIA): A (1.7%, no motor/sensory or sacral sparing), B (5.1%, sensory only, no motor below lesion), C (25.9%, 50% muscles less than Grade 3 below lesion), D (76.2%, 50% muscles more than Grade 3 below lesion), E (100% intact motor/sensory)
Specific evaluation
- Prolapse: vaginal (up to 33%) and rectal (up to 32%) seen over 5-6yrs follow up for both genders
- Stones: kidney stones seen in 34-64% SCI patients, bladder stones in up to 23% SCI patients and 8-41% chronic catheter patients
- Catheter exam: assess for bladder neck incompetence in women, traumatic hypospadias in men, SPT site bleeding (treat with silver nitrate)
AUA 2021 Guidelines Risk Recommendations
Risk Classification
- Low risk definition: suprapontine lesion, peripheral lesions, spontaneous voiding, low PVR, no hydronephrosis, no bladder stones, no UTI, normal renal function, no DSD (if assessed), stable voiding symptoms
- Unknown risk (determine moderate/high): suprasacral lesion, hydronephrosis, bladder stones, elevated PVR, recurrent UTI, worsening LUTS
- Moderate risk definition: UDS w/ BOO/retention/DO, elevated PVR, normal upper tracts, normal renal function
- High risk definition: UDS w/ poor compliance/elevated pressures w/ DO/DSD/VUR, hydronephrosis, new renal scarring, parenchymal loss, staghorn or increased stone burden, worsening renal function
Risk Surveillance
- Low risk surveillance: not indicated, reassess risk if new symptoms develop
- Moderate risk surveillance: annual H&P + renal function, upper tract imaging q1-2yrs, UDS as needed
- High risk surveillance: annual H&P + renal function + upper tract imaging, UDS as needed
- Surveillance after incorporating bowel: annual H&P, BMP, B12 (if ileum used), and renal US, consider cystoscopy if hematuria develops
References
- AUA Core Curriculum
- Cameron, M. D., et al. "The AUA/SUFU Guideline on Adult Neurogenic Lower Urinary Tract Dysfunction." (2021).
- Kowalik, C., A. Wein, and R. Dmochowski. "Neuromuscular Dysfunction of the Lower Urinary Tract." Campbell-Walsh Urology 12 (2020).
- Sakakibara, Ryuji, et al. "A guideline for the management of bladder dysfunction in Parkinson's disease and other gait disorders." Neurourology and urodynamics 35.5 (2016): 551-563.
- Solomon E, Yasmin H, Duffy M, Rashid T, Akinluyi E, Greenwell TJ. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourology and Urodynamics. 2018;37:368–378.