Causes of Neuromuscular Lower Urinary Tract Dysfunction
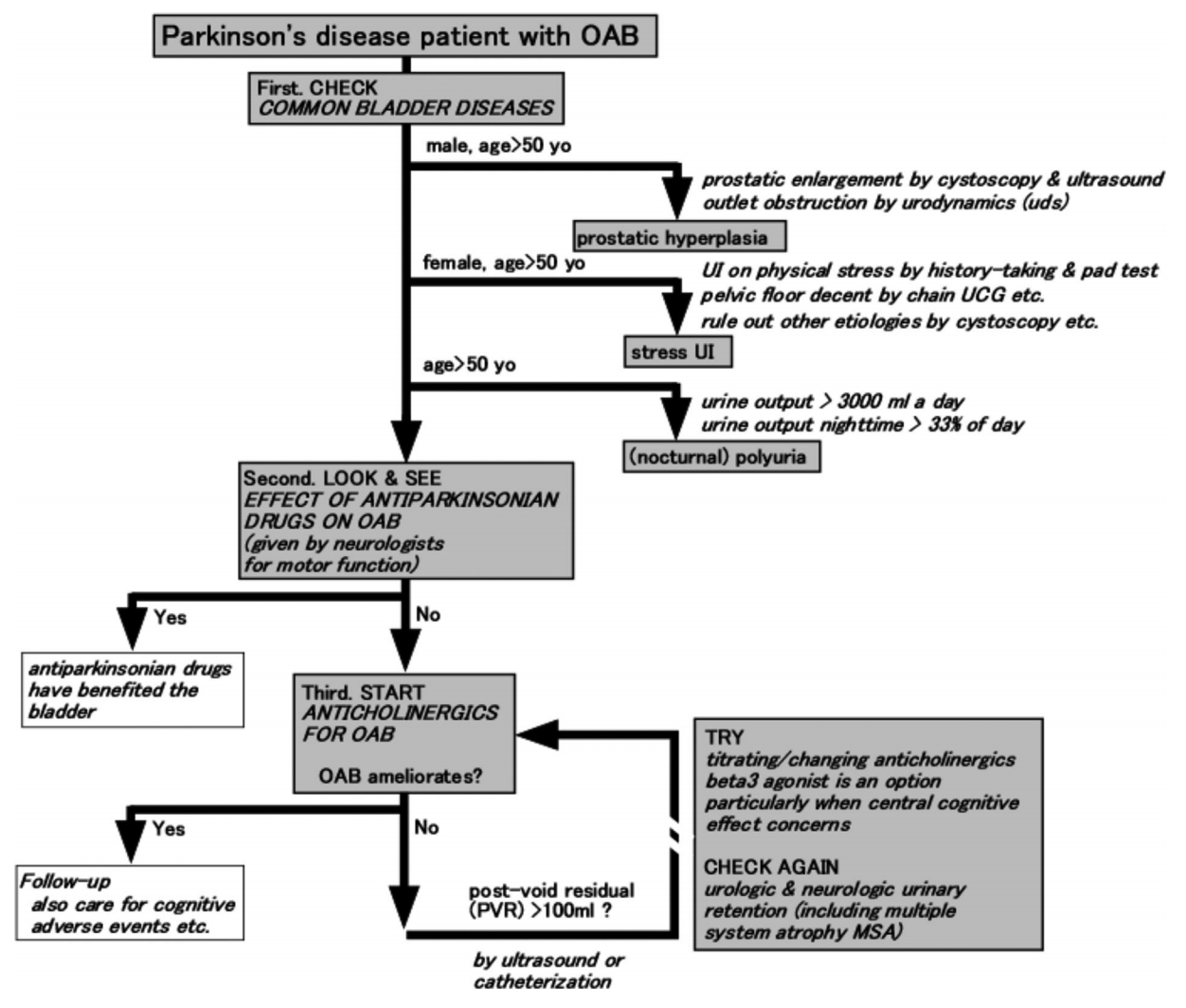
Workup of PD patient with LUTS, from Sakakibara 2016
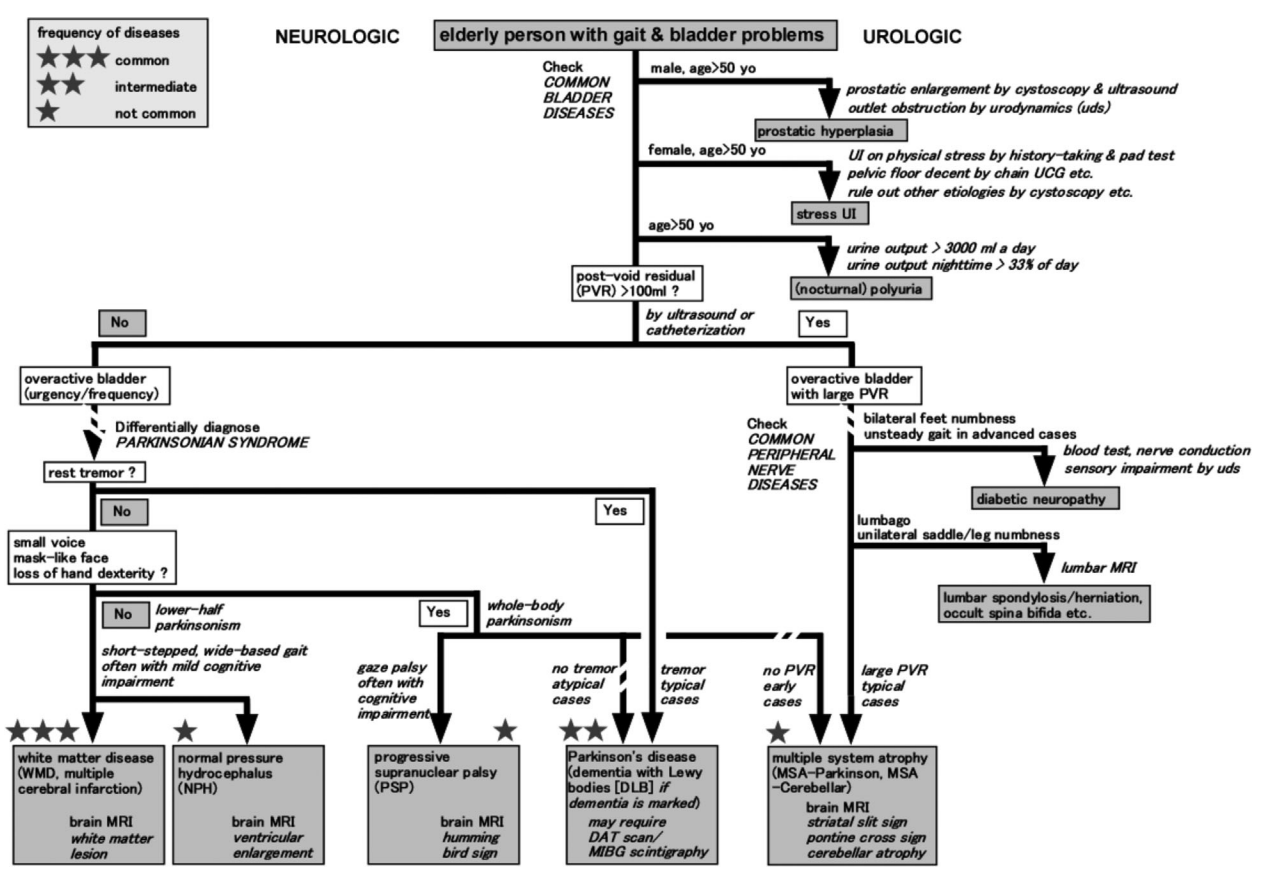
Diagnosing patients with LUTS and parkinsonism, from Sakakibara 2016
Cerebral diseases
Stroke (cerebrovascular accident)
- Urinary incontinence: 32-79% on admission, 25-28% on discharge, 12-19% months later, predictive of poor survival and functional independence (more than depressed consciousness), insensate incontinence more common (12-58% vs 9-42% sensate)
- Lenticulocapsular strokes more likely to cause incontinence (52% have incontinence)
- Relationship with fecal incontinence: both present (33%), urinary only (12%), fecal only (8%)
- Phasic detrusor overactivity: is most common post-CVA LUTD - 60-65% have DO, whereas 30-40% have DUA
- UDS indications: prior to BOO surgery to confirm cause of urinary symptoms
Parkinson Disease (PD)
- Pathophysiology: caused by dopamine deficiency in nigrostriatal pathway, presents with tremor + rigidity + bradykinesia
- Urinary symptoms: present in 35-70% - nocturia (86%), frequency (71%), urgency (68%)
- UDS findings: DO most common, true DSD is uncommon, pseudoDSD common due to bradykinesia, DUA uncommon
- Medications: urinary symptoms may be exacerbated by bromocriptine but not other medications
- Surgical intervention TURP (and other outlet surgery) is okay if Parkinson disease (not MSA), striated sphincter acontractility is rare, but obtain UDS to confirm
Parkinson+ syndromes
- Diagnoses: multiple system atrophy (MSA), progressive supranuclear palsy (PSP), corticobasilar ganglionic degeneration, vascular parkinsonism, Lewy body dementia
- PD vs parkinson+: combination of asymmetric symptoms, resting tremor, and response to L-dopa indicates likely PD
- Concerning findings: dementia, falls, symmetric symptoms, wide gait, normal eye movements, autonomic dysfunction
- Presenting symptoms: usually present with storage symptoms - nocturia, frequency, urgency
- Management: may require botox, sacral neuromodulation
Multiple system atrophy (MSA)
- Urologic findings concerning for MSA over PD: LUTS prior to parkinsonism, incontinence, elevated PVR, erectile dysfunction, and abnormal sphincteric function on EMG
- Symptoms may be parkinsonian dominant (MSA-P) or cerebellar dominant (MSA-C)
- Urinary symptoms usually preclude parkinson symptoms, the opposite for PD
- Management difficult to treat, may require CIC, do not perform outlet procedure (sphincteric incompetence)
Traumatic Brain Injury
- Urodynamics findings: DUA common in acute setting, transitions to DO with synergic sphincter activity, DSD may be present if pontine micturition complex (PMC) is damaged
- Incontinence: more common with poor functional status and bilateral lesions
- Retention: more common if diabetes or fecal impaction
Other diseases
- Brain tumor: variety of presentations, more associated with area affected than tumor type
- Cerebellar ataxia: poor movement coordination, presents with retention and DO but usually sphincteric synergy
- Normal pressure hydrocephalus (NPH): dementia + ataxia + incontinence, caused by DO + sphincteric synergy, treatment (VP shunt) shold improve incontinence
- Cerebral palsy: nonprogressive brain injury causing neuromuscular disability, most patients have normal storage/emptying, but voiding symptoms warrants UDS to rule out high pressure bladder, conservative management can be used for most
- Dementia: incontinence is common but unclear if abnormal mechanism or just poor awareness, anticholinergic use may exacerbate symptoms (brain loss of cholinergic neurons)
Spinal cord diseases
Multiple sclerosis (MS)
- Symptoms: 50-90% have LUTS, 37-72% have incontinence
- UDS findings: DO (34-99%), DSD (30-65%), DUA (12-38%)
- Factors predicting urologic complications: DSD in men, high filling pressures, and indwelling catheters
- Renal injury: rare, < 10% require surgical intervention for medication failure
- Management: medications + CIC (57%), medications (13%), CIC (15%), behavioral therapy, 50% have DSD improvement with a-blockers, avoid irreversible treatments (MS symptoms may change with flares and disease progression)
Spinal cord injury (SCI)
- 43% have incontinence, 7% have kidney stones within 10yrs injury (greatest risk within first 3mo after injury)
- Spinal shock: bladder becomes areflexic immediately after injury, striated sphincter does not close during filling (absent guarding reflex), no voluntary control, incontinence only occurs with overflow, manage with catheterization, lasts usually 6-12 weeks but up to 1-2yrs
- Suprasacral SCI: DO, DSD, smooth sphincter synergia
- Sacral SCI: DUA with varying compliance, nonrelaxing smooth sphincter and fixed striated sphincter
- DSD: causes functional obstruction, poor emptying, high detrusor pressures
- Treat based on symptoms and urodynamic findings, which may (not) correlate
- Asymptomatic bacteruria: common, only treat if signs/symptoms of UTI, prophylaxis warranted for rUTI without underlying cause, not warranted for ongoing catheter usage
- Bladder cancer: similar risk to general population but more likely to be muscle-invasive at diagnosis, unclear evidence for screening cystoscopy (or timing) but no other options currently available
- Follow-up: annually for at least 5-10 years after injury, check renal/bladder US, PVR (if applicable), and BMP
Spina bifida
- May have vertebral defects or meningeal sac herniation with(out) cord or nerve root evagination
- Urodynamic findings: DUA, open bladder neck, overflow incontinence, stress incontinence, DSD only seen in 10-15%
- Management: CIC/catheter, bladder augment, diversion, slings, botox, anticholinergics
- Tethered cord: presents with lower extremity weakness, sensory loss, bowel/bladder incontinence, treat based on urodynamic findings, post-treatment improvement seen in 95% within 6 months
Other diseases
- Cervical myelopathy: caused by cord compression, majority have some form of voiding symptoms
- Acute transverse myelitis: acute onset with variable recovery, variety of residual urinary deficits
- Tabes dorsalis (syphilitic myelopathy) and pernicious anemia: insensate bladder with DUA
- Polio: retention, DUA, intact sensation, seen in 4-42%
Lower motor neuron diseases
Lumbar disc disease
- Cauda equina compression: may occur in 1-15% due to central prolapse (as opposed to posterolateral)
- Pre-laminectomy urodynamics: may be warranted to determine whether voiding improves after surgery
- Cauda equina syndrome: perineal sensory loss with bowel/bladder incontinence, decompress within 48hr recommended, autonomic function usually slower to recover after surgery than somatic function
Spinal stenosis (narrowing of canal/foramina)
- Presents with back/extremity pain with exercise and relieved with rest
- Urologic symptoms: variable, ~50% improve after laminectomy, preoperative UDS may be helpful to determine improvement
Pelvic surgery
- Hypogastric plexus runs along rectum and vagina, can be injured during abdominoperineal resection (20-68%) and radical hysterectomy (16-80%)
- Prognosis: may be permanent in 15-20%, due to denervation, nerve tethering, bladder/urethral injury or devascularization
- Symptoms: presents with decreased bladder contractility, decreased compliance, fixed striated sphincter (decreased voluntary relaxation), open/nonfunctional smooth sphincter
- Management: CIC, monitor for improvement (may take 6-12mo)
Diabetes
- LUTD in 5-59%
- Incontinence: more likely urge than stress, 20% increased risk compared to non-DM
- Urodynamic findings: impaired bladder sensation, increased capacity, decreased contractility, decreased flow
- Management: encourage timed voiding to optimize emptying and prevent detrusor decompensation, may require CIC or SPT
Herpes
- Sacral nerve root infection can cause retention (DUA) within days-weeks after initial primary viral manifestations
- Can be secondary to genital or anal inefctions
- Cystoscopy may show bladder mucosa vesicles
- Elsberg syndrome: bilateral sacral nerve root involvement, leads to sphincteric incontinence and CSF pleocytosis
Guillain Barre Syndrome
- Presents with rapid limb weakness, loss of reflexes, and variable autonomic deficiencies
- LUTD seen in 25-80%, retention present in 11-30%
Voiding syndromes
Detrusor sphincter dyssynergia
- True DSD only exists in presence of neurologic injury/disease between brainstem (PMC) and sacral spinal cord
- Prognosis: untreated DSD leads to VUR, upper tract injury, stones, sepsis, and UVJ obstruction
- Management: decreasing abnormal sphincter activity (botox, sphincterotomy) or bypassing sphincter (CIC)
Dysfunctional voiding
- Involuntary sphincteric obstruction in the absence of neurologic disease, difficult to prove on UDS
- May be a response to discomfort with voiding or attempt to augment voiding
- Non-neurogenic urinary retention: PVR > 300mL for > 6mo, manage high risk patients (hydro, CKD, rUTI) with catheterization
Bladder neck dysfunction
- Incomplete opening during voiding
- Usually seen in younger men with chronic LUTS in absence of BPH on cystoscopy
- Diagnose via UDS which confirms outlet obstruction at level of bladder neck
- Management: a-blockers and TUIP (unilateral decreases risk of retrograde ejaculation)
- Smooth sphincter dyssynergia: UDS finding in patient with autonomic hyperreflexia
Female bladder outlet obstruction
- Urodynamic findings: non-neurogenic voiding dysfunction confirmed with videourodynamics showing obstruction between bladder neck and distal urethra
- Surgical treatment risks sphincteric incontinence
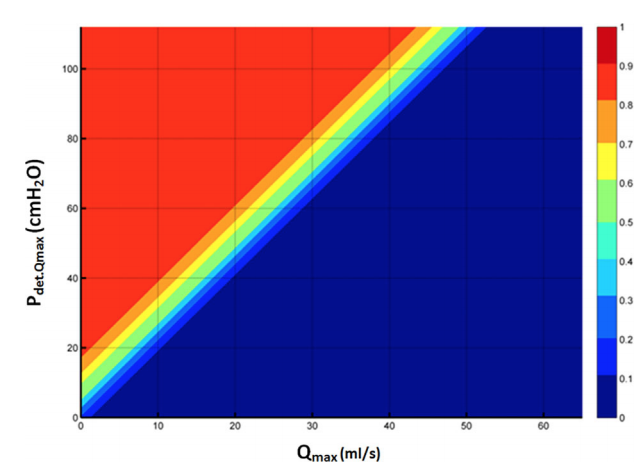
- New Solomon-Greenwell nomogram helps predict BOO
Bashful bladder (low-flow voiding)
- May be due to detrusor hyperactivity with impaired contractility, leading to frequency + hesitancy + poor stream
- Minimal additional diagnostic benefit to using ambulatory UDS
- Management: behavioral modification, usually no benefit to surgery
Fowler syndrome
- Definition: urinary retention in younger women in absence of neurologic disease
- Presentation: infrequent urination, abdominal discomfort, no urgency or sensation to void
- Management: responds best to neuromodulation (up to 70% success)
Post-operative urinary retention
- Contributing factors: foley trauma, overdistension, decreased sensation/contractility, increased outlet resistance, pain reflex, pre-existing obstruction
- Postoperative catheter drainage: improves postoperative retention risk compared to CIC
- Alpha blockers: unclear benefit to preop/postop a-blocker initiation
Irradiated bladder
- Storage symptoms: common within 4-6 weeks of XRT, return to normal within 6 months
- Delayed symptoms: late effects are uncommon but can be progressive and irreversible, due to tissue fibrosis
Defunctionalized bladder
- Urodynamic findings: decreased capacity, involuntary contractions, decreased compliance
- Can treat with cycling with increasing volumes
- Transplant safety: renal transplant is safe if capacity > 100mL and voiding pressure < 100cm
References
- AUA Core Curriculum
- Cameron, M. D., et al. "The AUA/SUFU Guideline on Adult Neurogenic Lower Urinary Tract Dysfunction." (2021).
- Kowalik, C., A. Wein, and R. Dmochowski. "Neuromuscular Dysfunction of the Lower Urinary Tract." Campbell-Walsh Urology 12 (2020).
- Sakakibara, Ryuji, et al. "A guideline for the management of bladder dysfunction in Parkinson's disease and other gait disorders." Neurourology and urodynamics 35.5 (2016): 551-563.
- Solomon E, Yasmin H, Duffy M, Rashid T, Akinluyi E, Greenwell TJ. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourology and Urodynamics. 2018;37:368–378.