Detrusor Underactivity
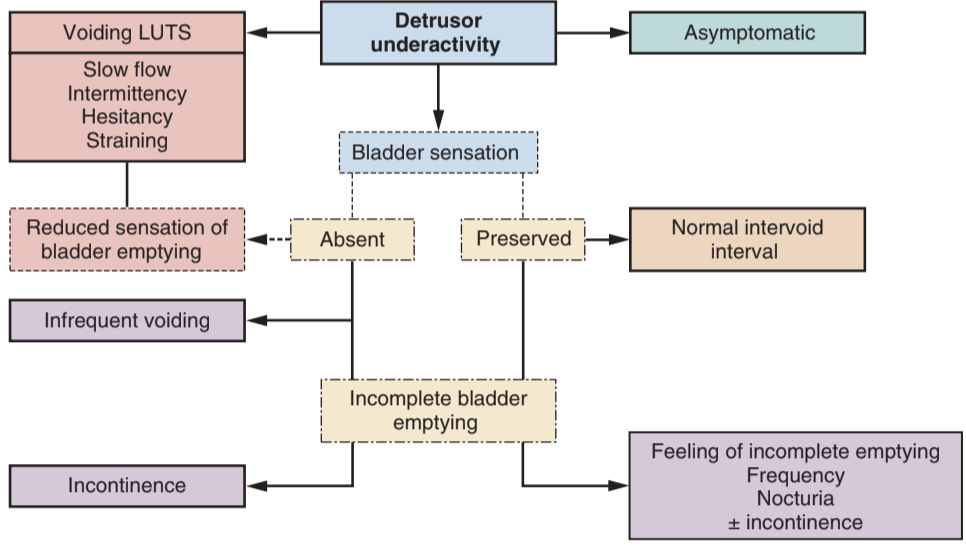
Symptomatic presentation of DUA, from Campbell's

Spectrum of DUA pathophys, from Campbell's
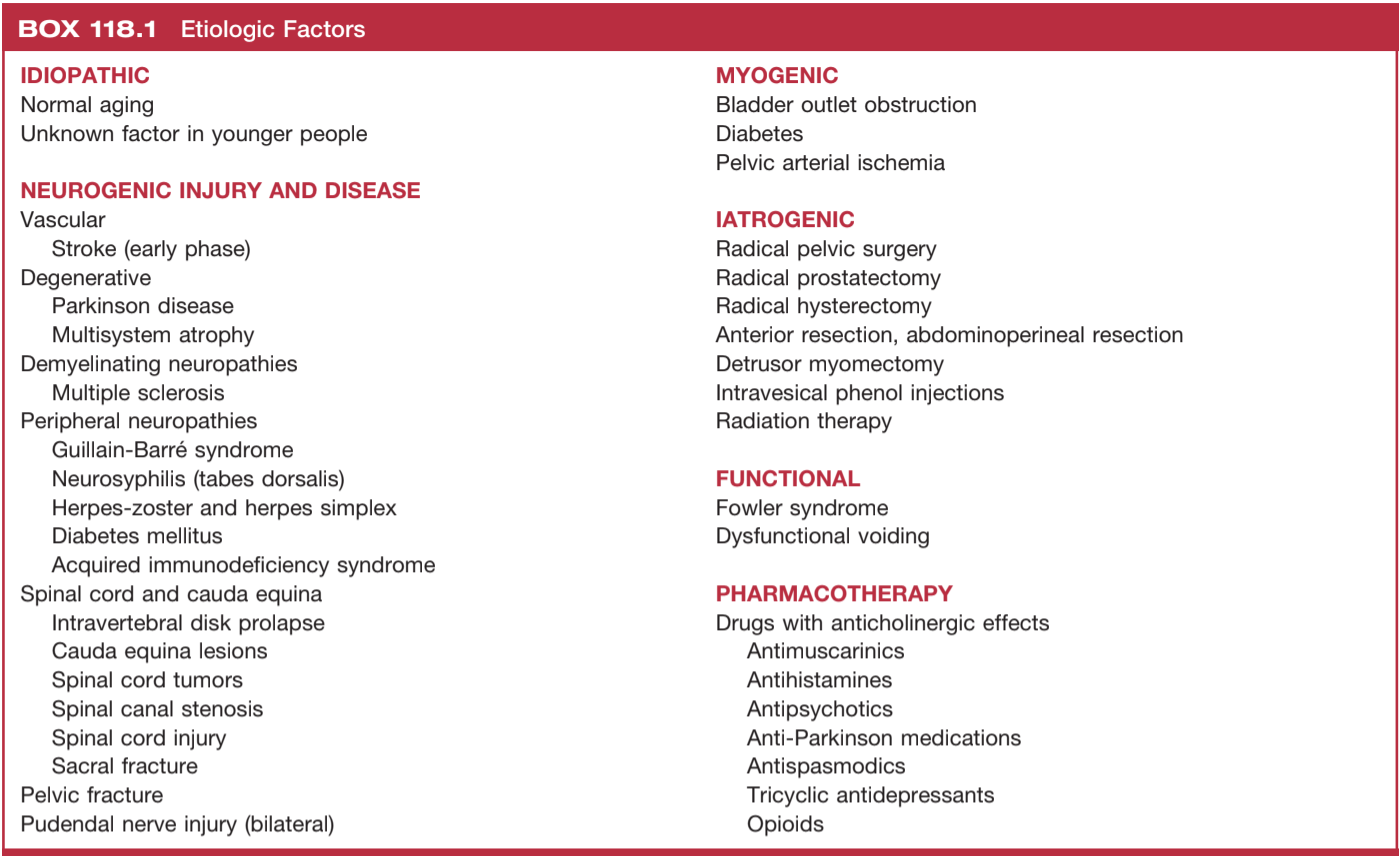
DUA Causes, from Campbell's
Presentation/Causes
- Symptoms: similar to BOO - straining, hesitancy, frequency, incontinence, nocturia
- DUA can be myogenic, neurogenic, or both, make sure to rule out undiagnosed neurologic causes
- Diabetic cystopathy: decreased bladder sensation (neuropathy) + myocyte dysfunction
- Iatrogenic: common after GYN/CR surgery, but most regain function within 1yr
- Urodynamics: the only way to definitively diagnose DUA
Treatment
- Behavioral: timed voiding, double voiding
- PFPT: 24% demonstrate improvement
- Valsalva/Crede: not recommended, can lead to prostatic/upper tract reflux
- CIC: preferred over indwelling catheter, offer SPT if unable/unwilling to self-catheterize
- Bethanechol: parasymathomimetic agent, no proven benefit, significant side effects (nausea, bronchospasm, GI distress), rarely cause cardiac arrest, not recommended
- a-blockers: may show some improvement in some patients (~30%)
- Sacral neuromodulation: FDA-approved for non-neurogenic causes of DUA, offer to motivated patients without severe comorbidities
- BOO surgery: up to 30% patients show improvement after BOO surgery despite no obstruction seen on urodynamics, patients require adequate counseling of questionable benefit prior to offering surgery, consider suprapubic tube placement as backup option
References
- AUA Core Curriculum
- Chapple, C., S. Ohlander, and N. Osman. "The Underactive Detrusor." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.