Benign Prostatic Hyperplasia Evaluation
Technically, benign prostatic hyperplasia (BPH) is a histologic diagnosis. BPH leads to benign prostatic enlargement (BPE), leading to bladder outlet obstruction (BOO), leading to lower urinary tract symptoms (LUTS).
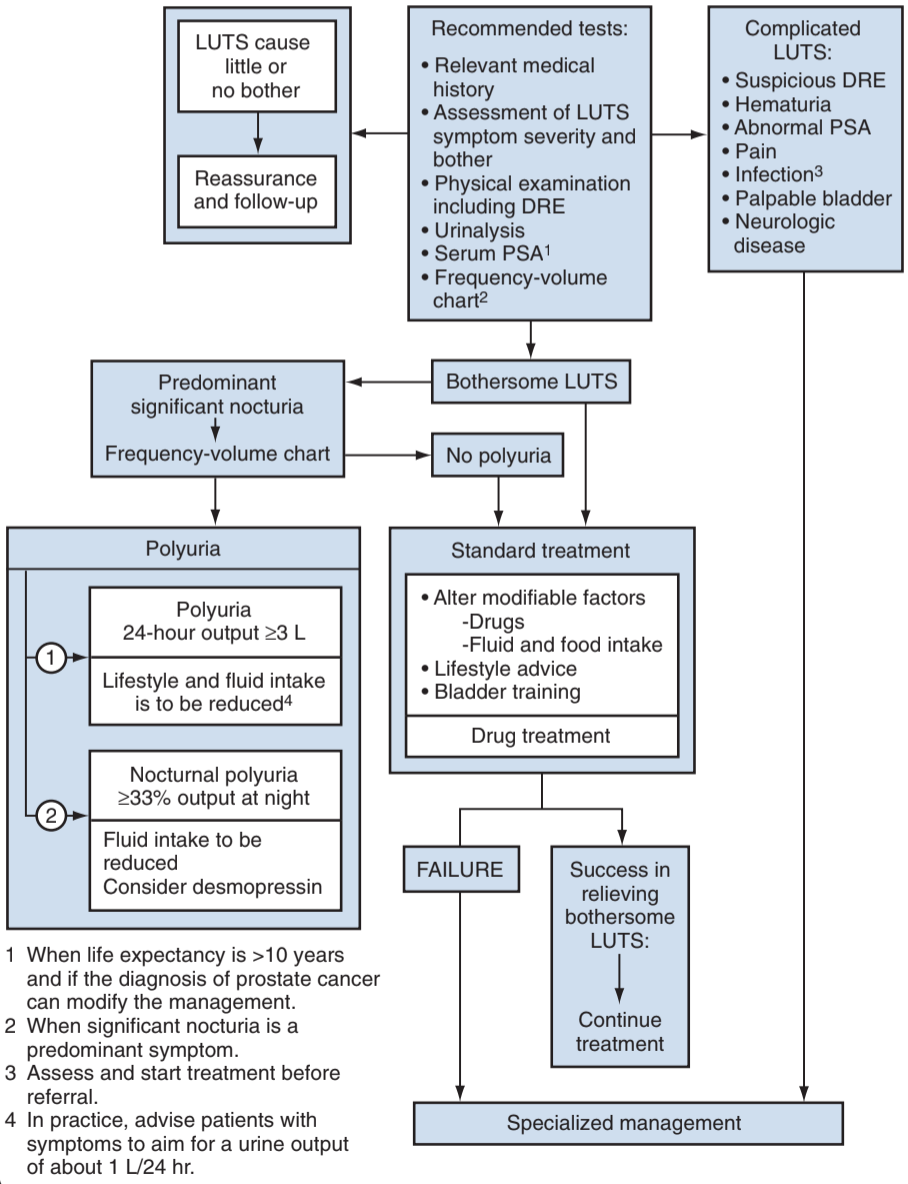
Evaluation/Workup
History
- Assess baseline symptoms: (voiding + storage), use AUASS
- Common conditions causing LUTS: DM, neurologic, CKD/CHF, OSA, cancer
- Fluid intake: assess amount and timing
- Bladder irritants: caffeine, alcohol, spicy food, acidic food
- Medications: a-agonists, anticholinergics
Clinic tests
- DRE: prostate cancer PPV 6-33%, poor estimate of prostate size
- PVR: no standardized definition or unified cutoff, questionable association with developing acute retention
- Uroflow: inaccurate if < 125-150mL, cannot distinguish BOO from DUA, consider 15mL/s a reasonable cutoff
- Cystoscopy: consider for gross hematuria, history bladder cancer, history recurrent UTIs or urethral injury, history prior urethral surgery, and prior to surgical planning, cannot accurately predict prostate size
- UDS: recommended if prior surgical therapy, unable to void > 150mL, PVR > 300mL, concern for neurologic disease, prior pelvic surgery, age > 80 or < 50 and predominantly voiding symptoms
BPH Labs
- UA: may be helpful for identifying UTI or hematuria
- Cytology: consider if severe storage symtpoms, dysuria, and smoking history
- PSA: consider checking after discussing risks/benefits and need for further workup, only check if cancer diagnosis will change BPH management (life expectancy > 10yrs)
- Renal fxn: check if considering surgical management (increased postop risks)
References
- AUA Core Curriculum
- Capogrosso, P., A. Salonia, and F. Montorsi. "Evaluation and Nonsurgical Management of Benign Prostatic Hyperplasia." Campbell-Walsh Urology 12 (2020).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.