Upper Tract Infections
Pyelonephritis
Acute Pyelonephritis
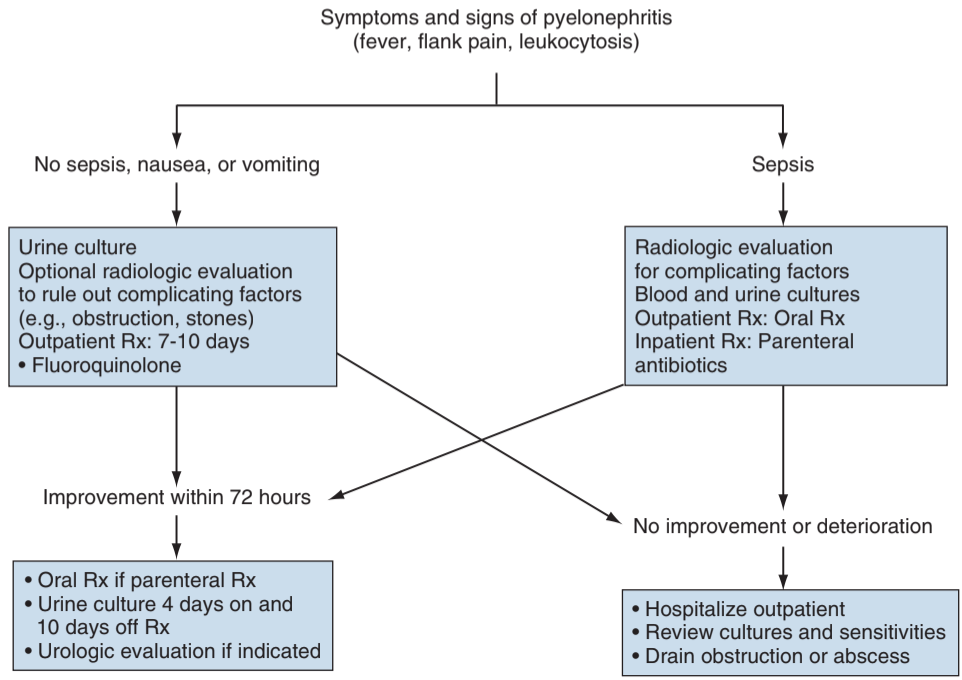
- Diagnosis: made clinically (not radiographically), fever + flank pain, lower urinary symptoms may (not) be present, DO NOT diagnose based on CT findings
- Complicated pyelonephritis: high fever, leukocytosis, vomiting, dehydration, sepsis, immunocompromised, male, DM
- Blood cultures: obtain in all men, or woman with systemic symptoms or risk factors
- Imaging: not required for diagnosis, can obtain renal US to assess for stones/hydronephrosis, CT warranted in patient with systemic symptoms or presumed complicated pyelonephritis, also obtain CT if persistent fever and symptoms > 72hr despite antibiotics
- Uncomplicated management: can be treated outpatient with PO antibiotics (ciprofloxacin 500mg BID or levofloxacin 750mg QD x1 wk +/- IV ceftriaxone 1g x1 or aminoglycoside x1)
- Complicated management: admit and give IV antibiotics (fluoroquinolone, aminoglycoside +/- ampicillin, cephalosporin or extended spectrum penicillin +/- aminoglycoside, carbapenem), treat with 2 weeks abx once cultures result
- "Test of cure" UCx: recommended, 10-30% will relapse after initial abx course, consider repeat 2-6wk course
Acute Focal/Multifocal Bacterial Nephritis
- Definition: infection of parenchyma creases inflammatory mass(es) without abscess, likely transition between pyelonephritis and renal abscess, approximately 1/4 patients will progress to renal abscess
- Symptoms: severe pyelonephritis symptoms, lower tract symptoms may be absent if hematogenous spread (IV drug use or cutaneous infection)
- Diagnosis: CT with contrast shows area of decreased enhancement, nephromegaly, decreased contrast uptake
- Management: obtain BCx/UCx, admit and start IV antibiotics, given antibiotics for 2+ weeks, reimage if no improvement within 72hrs to assess for abscess or obstruction
- VCUG: up to 50% have reflux, may benefit from workup after treatment of initial infection
Chronic pyelonephritis
- Diagnosis: atrophic/poorly functional kidney from prior episodes pyelonephritis, diagnosed radiographically (not clinically)
- Management: avoid UTI risk factors, control HTN
- Nephrectomy indications: normal contralateral kidney and affected kidney causing pain, symptomatic infections, or renin-mediated HTN
Emphysematous Pyelonephritis
- Definition: severe parenchymal infection with gas-forming infection
- Risk factors: diabetes + obstruction
- Mortality rate 19-43%
- Presentation: fever, vomiting, flank pain
- Diagnosis: made by demonstrating air in renal parenchyma on CT imaging
- Antibiotics: 3rd-gen cephalosporin + aminoglycoside (or carbapenem + vancomycin if concern for cephalosporin resistance)
- Management: glucose control, treat w/ drain(s) placement, consider nephrectomy only if extensive gas w/ renal destruction (25% mortality rate)
- Emphysematous pyelitis: air in collecting system only, treat with antibiotics + foley drainage (no need for stent/PCN)
Xanthogranulomatous pyelonephritis (XGP kidney)
- Definition: chronic infection destroying parenchyma, can locally extend through parenchyma and through Gerota fascia into retroperitoneum and adjacent organs
- Presentation: flank pain, fever, persistent bacteruria, anemia, 60% have a flank mass
- CT triad: present in 50-80% patients, unilateral enlargement + little/no function + large stone in renal pelvis
- Malignancy: often cannot distinguish XGP from malignancy, may require nephrectomy for confirmation
- Diagnosis: can only be made with pathology specimen, shows accumulation of lipid-filled macrophages
- Management: usually requires nephrectomy (often difficult due to severe inflammation), imaging may underestimate degree of inflammation and adjacent organ involvement, give vaccinations prior to L side nephrectomy (in case splenectomy required), can attempt treating stones with PCNL to salvage residual function
- Antibiotic coverage: > 4wks abx prior to surgery decreases length of stay and complication risks (per Xie 2021)
Abscesses and Pyonephrosis
Renal Abscess
- Presentation: fever, chills, abdominal/flank pain, weight loss, cystitis, may have flank mass, 50% have positive blood cultures
- Risk factors: DM (50%), rUTI (65%)
- Management: if < 3-5cm (depending on reference) treat with antibiotics and observe, otherwise drain percutaneously if larger or patient is clinically unstable or immunocompromised
Perinephric and paranephric abscesses
- Perinephric abscess: abscess outside renal capsule but contained within Gerota fascia, can be caused by abscess rupture, extravasation of infected urine, or spread from another source
- Paranephric abscess: abscess outside Gerota fascia, extends from perinephric abscess or adjacent organ abscess
- Psoas abscess: presents with limping, pain on flexion and external rotation of hip
- Management: similar criteria/recommendations as for renal abscess
- Symptom course: usually have symptoms > 5 days, and remain febrile for longer than 4 days
Infected Hydronephrosis +/- Pyonephrosis
- Infected hydronephrosis: bacterial infection in a hydronephrotic kidney
- Pyonephrosis: infected of chronic hydronephrosis, leading to decreased renal function and parenchymal destruction
- Diagnosis: imaging shows hydronephrosis with abnormal fluid and fat stranding, urinalysis may not show abnormalities if completely obstructed
- Management: place stent or PCN, may require nephrectomy if symptoms do not resolve
References
- AUA Core Curriculum
- Cooper, K. L., G. M. Badalato, and M. P. Rutman. "Infections of the urinary tract." Campbell-Walsh-Wein Urology. 12th ed. Elsevier (2020): 1129-1201.
- Koch, George E., and Niels V. Johnsen. "The Diagnosis and Management of Life-Threatening Urologic Infections." Urology (2021).
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.
- Xie, Lillian, et al. "Long-term antibiotic treatment prior to laparoscopic nephrectomy for Xanthogranulomatous pyelonephritis improves postoperative outcomes: results from a multicenter study." The Journal of Urology 205.3 (2021): 820-825.