Genital Infections
Balanitis + Balanoposthitis
Presentation
- Risk factors: poorly controlled diabetes (most common), poor hygiene, recent antibiotic use
- Complications from untreated disease: phimosis, lichen sclerosus, leukoplakia, meatal stenosis
- Presentation: pain, pruritus, rash, exam with erythema, fissures, ulceration, discharge, phimosis
- Workup: often treat empirically, can swab if concerned for fungal, Tb, Trichomonas, syphilis, HSV, test for DM and HIV if recurrent disease, can consider biopsy if symptoms do not resolve within 6 weeks
Management
- Conservative management: foreskin hygiene with cleaning and daily retraction
- Steroids: consider hydrocortisone 1%, can cause skin atrophy/discoloration, may require dermatologic evaluation if symptoms don't resolve within 4-6 weeks
- Candida treatment: clotrimazole 1% BID or miconazole 2% BID or nystatin cream 100K U/g BID until symptoms resolve, fluconazole 150mg PO x1
- Anaerobic bacterial treatment: metronidazole 500mg PO BID x1wk, clindamycin 10mg/mL topical BID until symptom resolution
Soft tissue infections
Topical infections
- Scrotal cellulitis: most often caused by B-hemolytic Streptococcus, symptoms include redness, warmth, swelling, pain (no crepitus, bruising, or necrosis), clinically diagnosed (no biopsy/aspiration required), empirically treat for Streptococcus for 5+ days
- Folliculitis: treat with hygiene, remove irritants, topical anti-infectious agent
- Furunculosis: abscess associated with hair follicle, can use warm compress, may require incision/drainage if large
- Trichomycosis axillaris: corynebacterial infection of hair follicles with characteristic odor, associated with hyperhidrosis, treat with shaving and antibacterial soaps
- Ecthyma gangrenosum: cutaneous manifestation of pseudomonal sepsis, erythematous macules leading to a gangrenous ulcer, poor prognosis, treat with IV antibiotics and wound debridement
- Bite wound: Eikenella corrodens is normal flora in human mouth but can cause painful necrotic ulceration at bite site, treat with augmentin 1500mg daily until healing occurs
Abscesses
- Scrotal abscess: diagnosed with exam (fluctuance/induration) and/or scrotal US, perform incision/drainage then pack or place penrose drain, give IV antibiotics if concern about systemic infection or patient is immunocompromised, treat empirically for Staphylococcus (most common cause)
- Pyocele: infection within tunica vaginalis, usually requires incision and drainage, may require orchiectomy if testis is infarcted/necrotic
- Periurethral abscess: can spread through Buck fascia and cause extensive infection, treat with SPT drainage and debridement
Fournier gangrene
- Risks: alcoholism, diabetes, cancer, malnutrition, trauma, PVD
- Presentation: rapidly progressing cellulitits leading to ischemia and necrosis, spreads along tissue planes (Dartos, Colles, Scarpa)
- Imaging: not required (clinical diagnosis), CT A/P (scan down to mid-thigh) to visualize parenchymal air
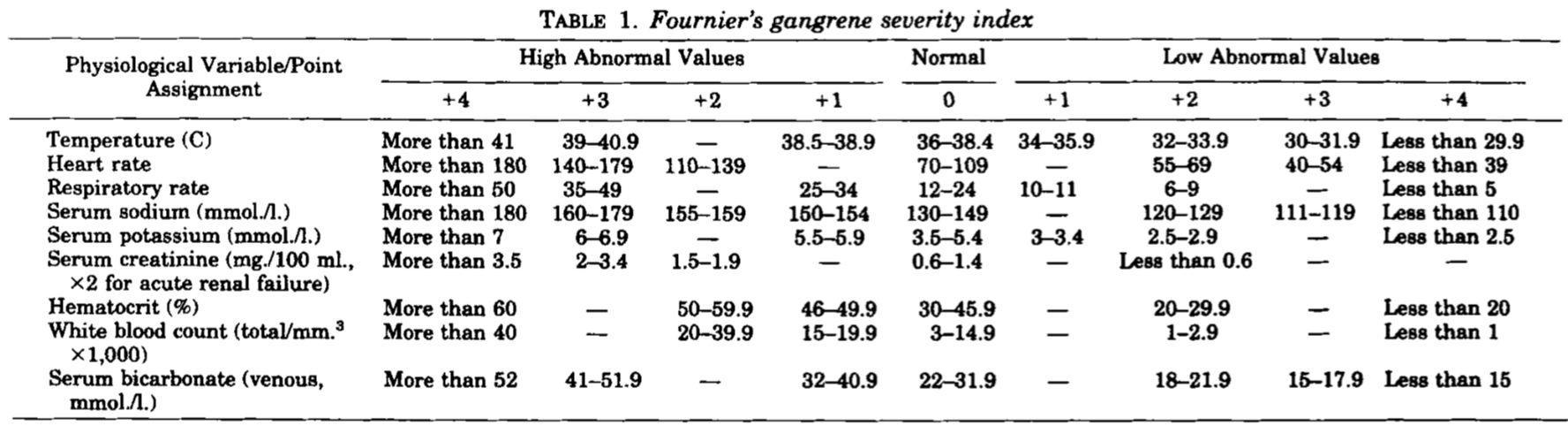
- Severity index: survival prediction tool (from Laor 1995), > 9 = 75% chance death vs ≤ 9 = 78% chance survival, although creatinine, hematocrit, and potassium seem to be the main predictors (Lin 2014)
- Initial treatment: wide surgical debridement, 2nd look within 48hr, consider SPT and colostomy, orchiectomy rarely required due to separate blood supply
- Reconstruction: cover skin defects with graft, suture testes together to prevent bifid scrotum formation
- Outcomes: mortality rate 5-40%, long-term sexual dysfunction ~65%
References
- AUA Core Curriculum
- Cooper, K. L., G. M. Badalato, and M. P. Rutman. "Infections of the urinary tract." Campbell-Walsh-Wein Urology. 12th ed. Elsevier (2020): 1129-1201.
- Koch, George E., and Niels V. Johnsen. "The Diagnosis and Management of Life-Threatening Urologic Infections." Urology (2021).
- Laor, Eliahu, et al. "Outcome prediction in patients with Fournier's gangrene." The Journal of urology 154.1 (1995): 89-92.
- Lin, Tsung‐Yen, et al. "Validation and simplification of Fournier's gangrene severity index." International Journal of Urology 21.7 (2014): 696-701.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.