Epididymoorchitis
Evaluation/Workup
Acute epididymoorchitis
- Non-infectious causes: tumors, Behcet disease (oral/genital ulcers, uveitis, skin lesions), amiodarone epididymitis, anti-sperm antibodies, trauma, torsion
- Infectious causes: E. coli, gonorrhea, chlamydia, mumps, coxsackie virus, Tb, fungus, ureaplasma, Trichomonas
- Potential symptoms: pain, swelling, urethritis/discharge, fever, hydrocele, erythema/edema on exam
- Workup: diagnosis and underlying cause made with history/physical, scrotal US can be beneficial but not required if diagnosis clear
- Infectious treatment: ceftriaxone 250mg IM x1 + doxycycline 100mg BID x10 days (if STI suspected), levofloxacin 500mg daily x10 days (if UTI suspected), ceftriaxone 250mg IM x1 + levofloxacin 500mg daily x10 days (if cause unclear)
- Further management: admit for IV antibiotics if fevers or leukocytosis, consider repeating imaging if no improvement within 72hrs, induration/swelling can takes weeks/months to resolve
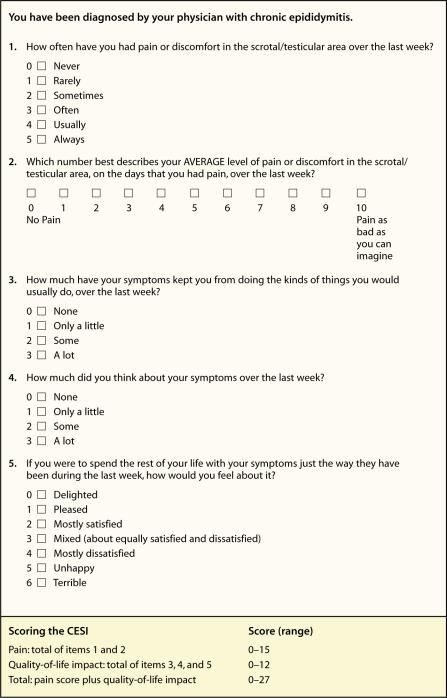
Chronic epididymoorchitis
- Definition: pain lasting for > 6 weeks
- Causes: post-surgical, pelvic floor dysfunction, post-infectious, granulomatous, amiodarone, tumor, varicocele, referred pain (stone, hernia, herniated disc, aortic aneurysm), may be idiopathic (18-25%)
- Post-vasectomy: 30% report short-term pain, chronic pain in 0.1-15%
- Granulomatous: can be infectious (TB, brucellosis, syphilis, leprosy), post-BCG, sarcoidosis, or idiopathic, may require orchiectomy to differentiate from malignancy
- Workup: culture urethral discharge (if present), scrotal US (assess for testicular abnormalities), can consider CT imaging to assess for causes of referred pain
- Conservative management: scrotal support, NSAIDs, avoid exacerbating activities, heat/ice packs
- BCG orchitis: isoniazid 300mg QD and rifampin 600mg QD x3-6mo, check LFTs and give Vitamin B6 50mg QD while taking isoniazid, do not need to treat if asymptomatic
Treatments
Minimally invasive therapies
- Pelvic floor physical therapy: consider if abnormal pelvic floor tone is noted on DRE and patient has other associated symptoms
- Cord block: inject 20mL 0.25% bupivicaine (without epinephrine) into spermatic cord, can also combine with methylprednisolone, resolution of pain indicates non-referred pain and cord denervation may be beneficial, testicular atrophy is rare but possible side effect
- Botox: inject 100U distal to external ring, wears off by 6mo
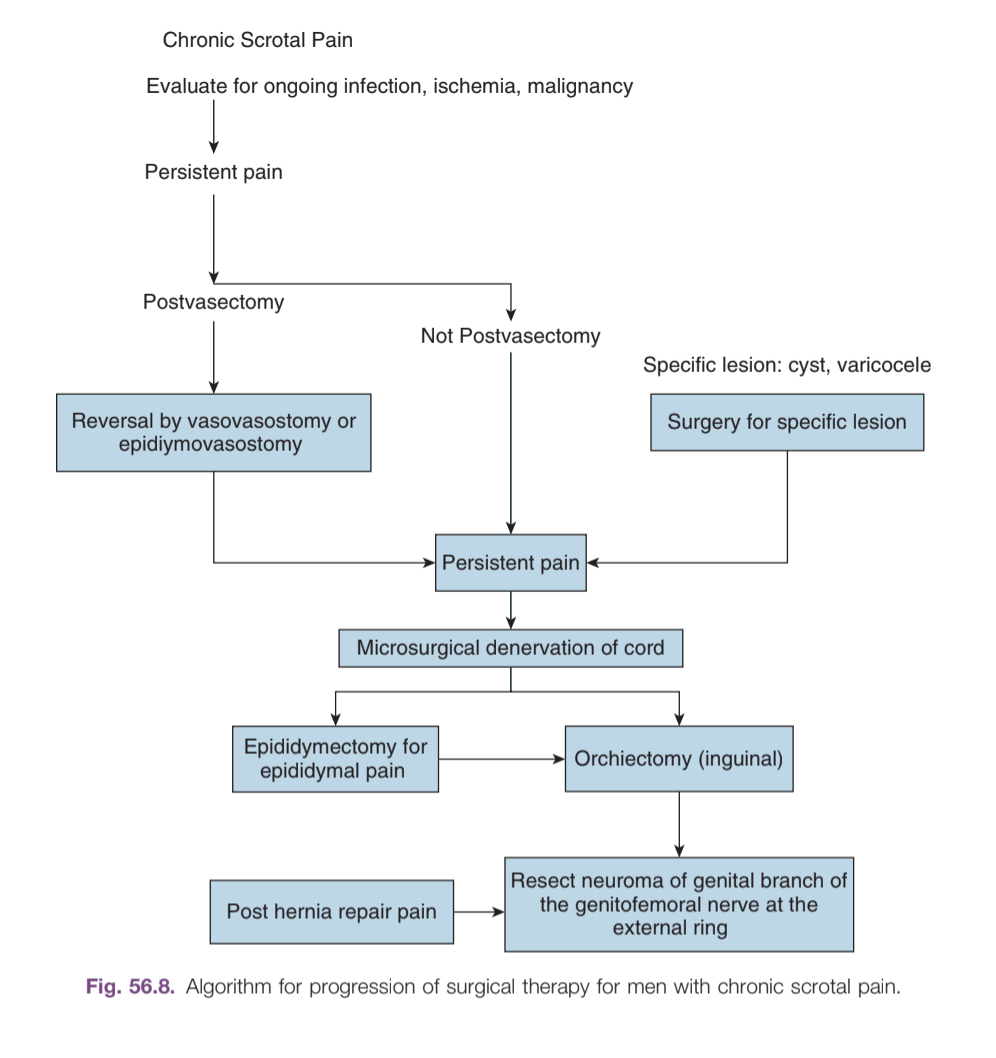
Surgical options
- Targeted excision: if pain is clearly due to hydrocele, spermatocele, torsion, patients report good improvement with repair
- Varicocelectomy: microsurgical (up to 85% pain resolution), nonmicrosurgical (up to 72%)
- Post-vasectomy pain: pain may be due to sperm granuloma, consider vasectomy reversal, may take 3mo to improve pain
- Cord denervation: transect nerves found in cremasteric muscle fibers, perivasal sheath, and posterior lipomatous tissue (trifecta nerve complex), cure rates 50-70%
- Neuromodulation: minimal data, only effective with case reports
- Epididymectomy: complete improvement in 50-75%, progression to orchiectomy in 22-100%
- Orchiectomy: relief in 0-75%, better improvement with inguinal approach
- Post-orchiectomy phantom pain: identify genital branch of genitofemoral nerve, resect neuroma, place proximal end into pelvis