Cutaneous GU Diseases
Allergic dermatitis, from Campbell's
Papulosquamous disease, from Campbell's

Vesicobullous disease, from Campbell's

Ulcers, from Campbell's
Autoimmune related dermatites
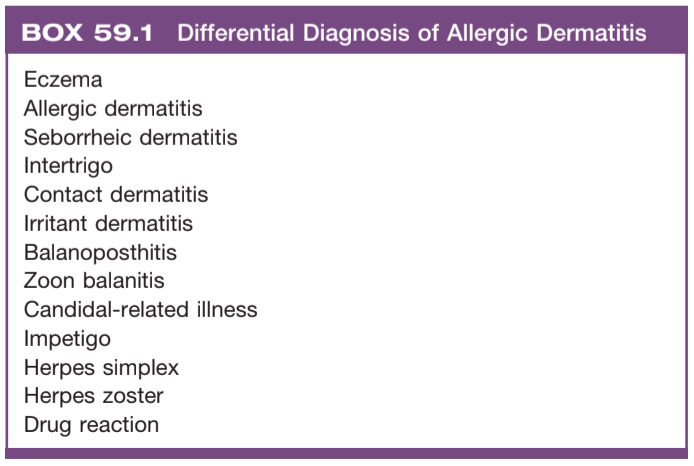
Allergic dermatitis
- Eczema: causes intense itching, usually with extragenital manifestations, associated with environmental triggers, treat topically with nonalkali soaps and emollients, orally with steroids, antihistamines
- Contact dermatitis: avoid exposure to irritants, may be caused by genital piercing, ask about products used on genitals
- Erythema multiforme: red papules that evolve into target lesions, most often seen with herpes infection
- Stevens Johnson syndrome: develop macules and blisters similar to severe burns, usually drug related, treat with systemic therapy, usually safe to place catheter and no need for cystoscopy
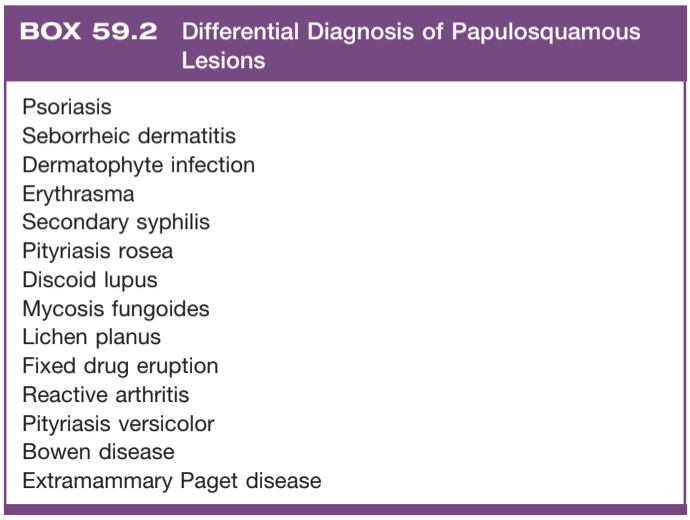
Papulosquamous disorders
- Psoriasis: sharply demarcated erythematous plaque with silvery scales, treat with short course topic steroids, do not treat genital lesions with UV therapy
- Reactive arthritis: urethritis + arthritis + ocular findings + oral ulcers, occurs after STI or GI infection, more common in HIV+ patients, may have psoriaform penile lesions (balanitis circinata), treat with topical steroids
- Lichen planus: purple papules/plaques sometimes with ulceration, 2/3 spontaneously resolve within 1yr, treat with topical steroids
- Lichen nitidus: fleshy papules in clusters, most spontaneously resolve, treat with topical steroids
- Lichen sclerosus: tissue pallor and scarring, can cause phimosis and urethral strictures in men, can cause vulvar adhesions and vaginal obstruction in women, treat with topical steroids (clobetasol 0.05% BID), consider daily catheterization using steroid cream as lubricant for intraurethral manifestation, may require circumcision
- Seborrheic dermatitis: pigmented plaques with adherent scale, more common in uncircumcised patients, severe manifestations seen in underlying HIV, treated with topical antifungals (unclear if fungal origin)
Bullous diseases
- Pemphigus vulgaris: 50% have genital lesions, painful oral lesinos are characteristic, treat with systemic steroids
- Bullous pemphigoid: itching that becomes blisters, less common mucosal involvement than vulgaris, treat with systemic steroids
- Dermatitis herpetiformis: cutaneous manifestation of celiac disease, avoid gluten, may treat with dapsone
- Hailey-Hailey disease (benign familial pemphigus): rare, caused by abnormal cell adhesion, intertriginous itching, pain, and foul odor, avoid friction/sweating, treat with steroids
Ulcerative diseases
- Aphthous ulcers: usually seen in mouth (canker sores) but can appear on genitals, if seen together with uveitis consider Behcet disease, variety of severity in presentation
- Pyoderma gangrenosum: ulcers with purulent base, wide variety of underlying causes, genital involvement uncommon
Non-autoimmune diseases
Non-STI infections
- Balanitis: can involve the prepuce (balanoposthitis), treat with antibiotics and hygiene, may requiring cricumcision
- Cellulitis: treat to cover S. pyogenes and S. aureus, may need to mark zone of infection to assess for improvement
- Folliculitis: treat with hygiene, remove irritants, topical anti-infectious agent
- Furunculosis: abscess associated with hair follicle, can use warm compress, may require incision/drainage if large
- Trichomycosis axillaris: corynebacterial infection of hair follicles with characteristic odor, associated with hyperhidrosis, treat with shaving and antibacterial soaps
- Ecthyma gangrenosum: cutaneous manifestation of pseudomonal sepsis, erythematous macules leading to a gangrenous ulcer, poor prognosis, treat with IV antibiotics and wound debridement
- Bite wound: Eikenella corrodens is normal flora in human mouth but can cause painful necrotic ulceration at bite site, treat with augmentin 1500mg daily until healing occurs
- Candidal intertrigo: red pruritic skin with satellite lesions, treat with topical antifungal agent for 2+ weeks, may require oral agents, can use drying powders, consider workup for diabetes
- Dermatophyte infection (jock itch): caused by non-candidal fungal infection, sharply demarcated erythematous plaques with raised scaly border, keep areas dry, treat with topical antifungals (but do not treat postinflammatory hyperpigmentation seen in chronic infections)
- Pubic lice (Pediculosis pubis): can be seen in children without sexual contact, nits/lice usually visible, manage with permethrin 1% cream rinse (q1w x2 doses) or malathion 0.5% lotion, wash clothes/bedding in hot water or seal in a bag x3 days
- Scabies (Sarcoptes scabiei): rash/itching with serpiginous lines, manage with permethrin 5% cream or ivermectin 200ug/kg PO q2w x2 doses, wash clothes/bedding in hot water or seal in a bag x3 days
Benign conditions in men
- Fordyce spots: vascular ectasias, 1-2mm red/purple papules, can occasionally cause scrotal bleeding, can treat with laser therapy
- Pink pearly papules: whitish closely spaced papules usually seen around corona, seen in 14-48% men (more common if uncircumcised), unrelated to HPV, can treat with laser therapy, histologically angiofibromas
- Zoon balanitis: seen in uncircumcised men, papules/plaques on glans with shallow erosions, cured with circumcision or topical steroids
- Sclerosing lymphangitis: indurated/tender cord involving coronal sulcus and penile skin, usually associated with prior sexual trauma and resolves within weeks
- Median raphe cyst: seen on ventral portion of penis, do not communicate with urethra, treat with surgery
- Ectopic sebaceous glands: small flesh-colored papular lesions, pin sized, no treatment warranted
Non-gender specific benign conditions
- Skin tag: usually asymptomatic but can become painful from trauma or torsion, seen in areas of friction, can excise, may be confused for fibrofolliculomas
- Epidermoid cysts: nonpainful, seen everywhere including scrotum, can rupture and cause painful inflammatory reaction, excise entire cyst wall to prevent recurrence, may require I&D if infected
- Seborrheic keratosis: lesions with stuck-on appearance, may drop off and spontaneously regrow, can treat with excision, abrupt increase in number can be associated with internal malignancy (Leser-Trelat sign)
- Lentigo simplex: brownish macules unrelated to sunlight, usually smaller than melanocytic nevi, biopsy if abnormal appearing
- Dermatofibroma: small hyperpigmented nodule, pinching causes downward movement (dimple sign), excision may result in cosmetic appearance that is postoperatively worse than preoperative appearance
- Neurofibroma: skin colored rubbery nodules, pressure causes invagination (button-holing), multiple may indicate Neurofibromatosis
- Capillary hemangioma: can occasionally cause bleeding or obstruction, majority involute with time, can treat with propranolol or topical timolol
Hidradenitis suppurativa
- Definition: blocked apocrine glands in axilla and anogenital regions, plugged follicles rupture into dermis leading to abscesses and sinus tracts, infection appears secondary
- Presentation: inflammatory nodules and sterile abscesses in axillae/inguinal/genital regions, chronic and relapsing
- Hurley classification: abscesses without sinus tracts or scarring (Stage I), recurrent abscesses with sinus tracts or scarring (Stage II), diffuse involvement of multiple interconnecting abscesses (Stage III)
- Conservative therapy: smoking cessation, good hygiene, weight loss, minimize friction, DM control
- Pain: can become chronic issue, avoid narcotics, try NSAIDs (topical), neuromodulators
- Topical agents: clindamycin 0.1% BID x6-8w (does not treat underlying condition), resorcinol 15% x4-6w
- Oral agents: tetracycline 500mg or doxycycline 100mg BID (Stage I), rifampin 300mg BID + clindamycin 300mg BID (Stage II)
- Steroids: intralesional triamcinolone 10 mg/mL, PO prednisolone (10mg/d) x4-6w
- Immune modulators (anti-TNF): adalimumab (80mg qw x2 -> 40mg qw x24), infliximab (7.5-10mg/kg q4w)
- Surgical therapy: I&D only provides temporary relief, surgical excision has low recurrence rates (0%-37%), recurrence associated with degree of excision and not wound coverage (primary intent vs secondary intent vs flap vs STSG)
References
- Anduquia-Garay, Felipe, et al. "Hidradenitis suppurativa: Basic considerations for its approach: A narrative review." Annals of Medicine and Surgery 68 (2021): 102679.
- Link, R. and N. Tang. "Cutaneous Diseases of the External Genitalia." Campbell-Walsh Urology 12 (2020).
- Michel, Chloe, et al. "The treatment of genitoperineal hidradenitis suppurativa: a review of the literature." Urology 124 (2019): 1-5.
- Nesbitt, Emily, Stephanie Clements, and Marcia Driscoll. "A concise clinician’s guide to therapy for hidradenitis suppurativa." International journal of women's dermatology 6.2 (2020): 80-84.