Preoperative Care
Preoperative Evaluation
Labs and Adjunct Testing
- UA/UCx: recommended if expected entry into GU tract
- Coags: consider if on active anticoagulation, history coagulopathy, or history operative bleeding
- Pregnancy test: any premenopausal woman who could potentially be pregnant
- Type & screen: any patient undergoing abdominopelvic surgery or percutaneous renal access (increased transfusion risk)
- ECG: questionable benefit, consider for patients > 40yo or with history cardiac disease
- CXR: beneficial if history cardiopulmonary disease
- HbA1c: assess if diabetic, recommend delaying elective surgery if > 6.9
Organ-specific evaluation
- Cardiac: modified risk index helps to stratify risk, ability to complete 4+ METs indicates no need for further cardiac evaluation
- Pulmonary: comorbidities increase risk for complications, assess OSA with Berlin or STOP-BANGquestionnaires
- Hepatobiliary: MELD score may be helpful to predict surgical complications even in absence of liver disease
- ACS NSQIP risk calculator: helpful to assess patient surgical risks based on nationwide patient data, although for larger surgeries may underestimate risk, other calculators include RAI Frailty and UCSF UroARC for BPH/URPS procedures
Specific patient populations
- Age: independently increases morbidity/mortality, increased risk for hospital delirium
- Obesity: increased comorbidities and surgical complications
- Pregnancy: attempt to delay until baby delivered, otherwise attempt to perform surgery during 2nd trimester
- Malnutrition: consider TPN or enteral feeding to decrease surgical wound complications
- Smoking: stop 8+ weeks prior to surgery to achieve risk reduction, otherwise may actually increase complication risks
- Diabetes: discontinue long-acting hypoglycemics (meglitinides, sulfonylureas, SGLT-2i, acarbose) to prevent intraoperative hypoglycemia
- Hyperthyroid: increased risk for thyroid storm (treat with B-blockers, iodine, steroids), difficult airway (from goiter)
- Steroids: HPA suppression seen with 20+mg prednisone taken for 3+weeks, give 50-100mg IV hydrocortisone prior to induction, 25-50mg hydrocortisone q8hr for 24-48hr until baseline steroid use is resumed
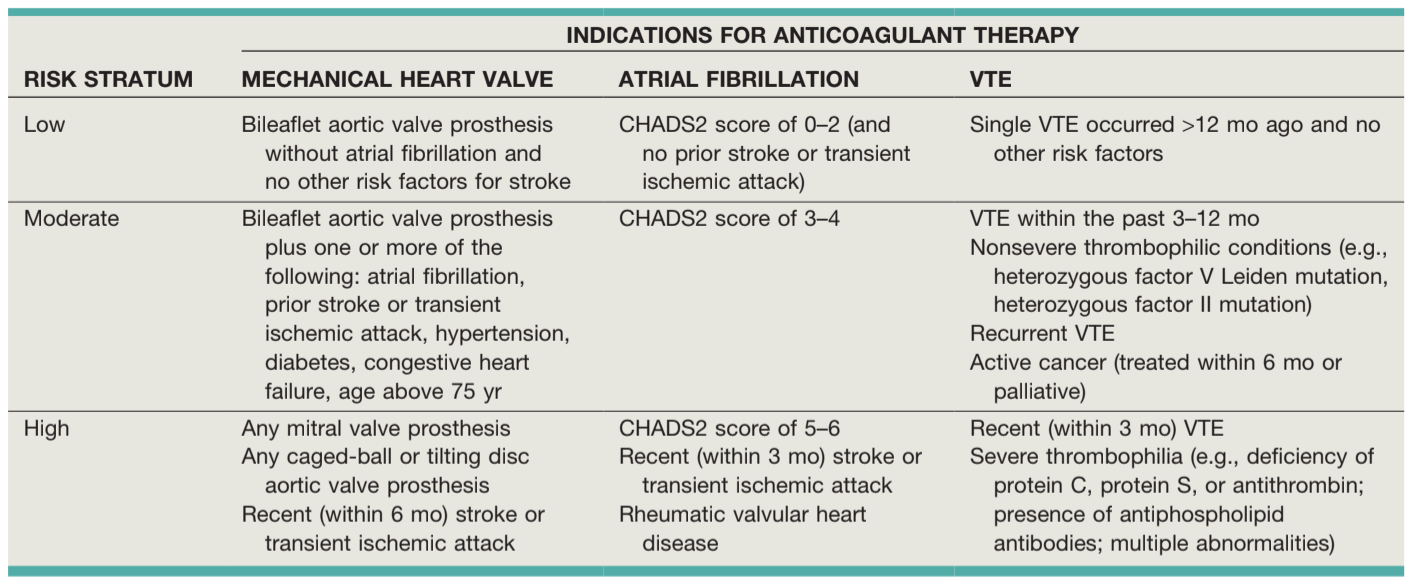
Anticoagulation
- Antiplatelet agents: require 7-10 days to reverse (14% normal platelet function restored per day)
- Do not need to discontinue low dose aspirin (ASA 81mg) prior to prostate biopsy, increased risk for minor bleeding
- Can perform ureteroscopy and laser prostate surgeries without stopping anticoagulation
- If on dual-antiplatelet therapy, try to continue aspirin if possible
- Moderate + high risk groups should undergo bridging (not safe to stop)
- Cardiac stents: wait 6-12 weeks for bare metal, 12mo for drug-eluting
- THE KEY: decision often made on individual patient situation, hematology/cardiology consults are recommended if continuing/stopping medications is unclear
- For high risk surgeries (cystectomy, RPLND), recommend preop dose SQH 5KU, discharge home with prophylaxis x4 weeks (recommended by NCCN but not AUA)
References
- AUA Core Curriculum
- Culkin, Daniel J., et al. "Anticoagulation and antiplatelet therapy in urological practice: ICUD/AUA review paper." The Journal of urology 192.4 (2014): 1026-1034.
- Naik, Rishi, et al. "The role of extended venous thromboembolism prophylaxis for major urological cancer operations." BJU international 124.6 (2019): 935-944.
- Stoffel, J. T., et al. "Optimizing outcomes in urologic surgery: preoperative care for the patient undergoing urologic surgery or procedure." (2019).
- Violette, Philippe D., et al. "Guideline of guidelines: thromboprophylaxis for urological surgery." BJU international 118.3 (2016): 351-358.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.