Catheter Placement and Troubleshooting
Catheter types and indications
- Coude: upwards curve helps maneuver prostate, larger size (18+) better otherwise catheter will buckle
- Silicone: stiffer catheters help navigate strictures and blind placement with severe phimosis, smaller size (12Fr) works best
- Council: hole at tip to pass over wire after dilating urethral stricture
- Hematuria: stiffer material allows for irrigation of large clots without collapsing during aspiration, 3-way for continous bladder irrigation
Placement tips
- Relaxation: taking slow deep breaths in via nose out via mouth helps relax sphincter and makes placement easier
- Lubricant: injecting directly into meatus improves placement but may initially clog drainage hole (need to flush)
- Lube temp: cooling in cup with ice helps decrease discomfort
- Hubbing: ensure hubbed completely prior to inflating balloon (avoids inflating in prostatic urethra)
- Urine level: if air/fluid level moves with patient respirations, catheter is adequately placed in bladder
- Female position: trendelenberg, frog-leg, pillow under hips, retract labia up and outwards
- Female urethral identification: under pubic bone (retracts into vagina with aging), can blindly slide catheter over finger in vagina, coude may help
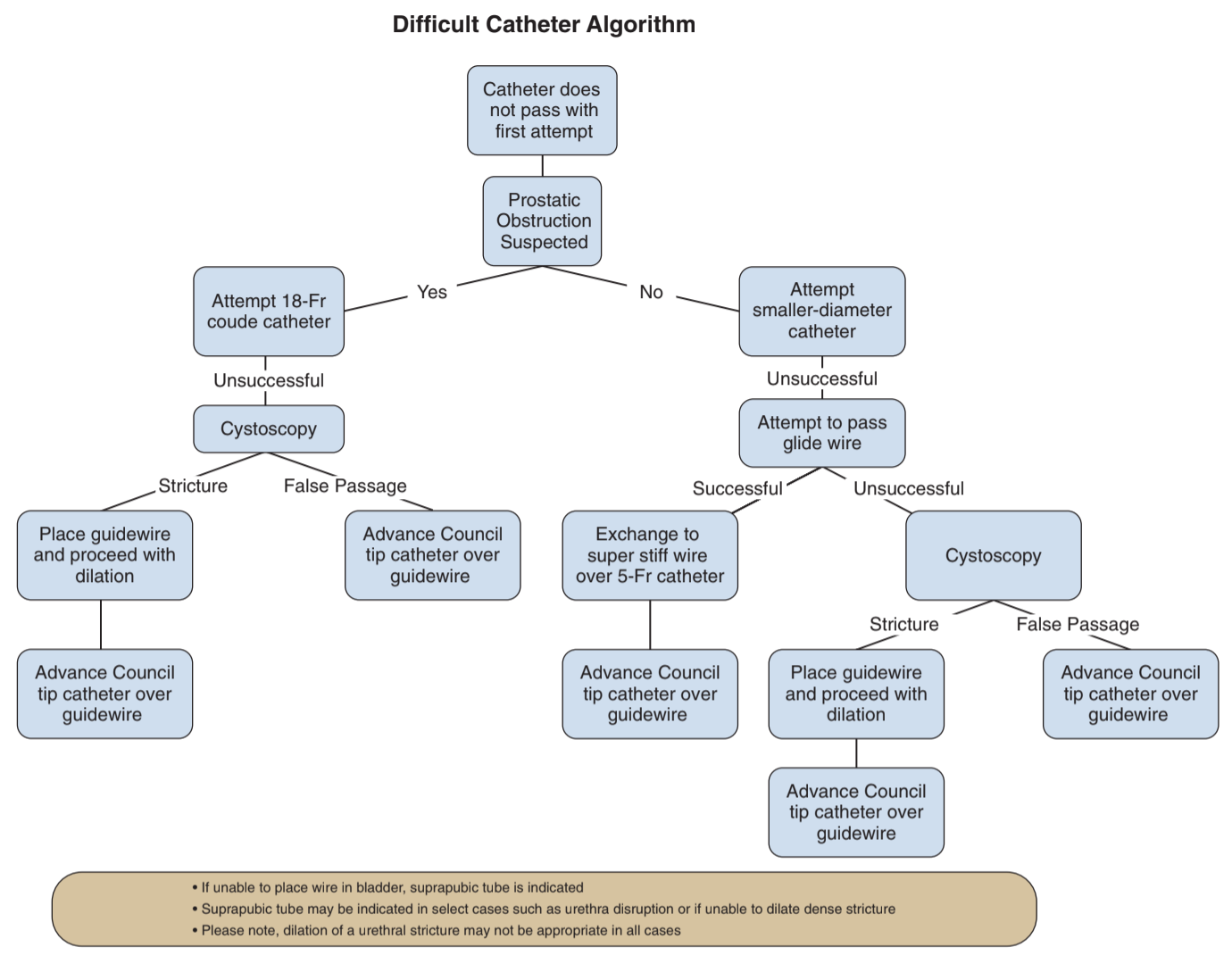
Difficult situations
- History: assess prior abdominal surgeries, urethral stricture disease, prior prostatic/bladder surgeries
- BPH: use coude, larger sizes pass more easily (18Fr > 12-14Fr)
- Stricture/phimosis: use silicone (stiffer), smaller size (12-14Fr), can blindly place through foreskin into meatus
- Concern for false passage: have concern if no urine return or blood at catheter tip, may require cystoscopy, false passage usually posterior and true lumen more anterior
- Difficult stricture: attempt placement of open ended catheter and wire, otherwise visualize stricture directly with cystoscope, then use dilators (straight or S-shaped) over stiff wire before placing Council, dilate 2 sizes greater than catheter, council catheter may not be stiff enough (use silicone with hole punched in end)
- Buried penis: pressure on surrounding tissue exposes penis, otherwise may have to place blindly or use cystoscope to identify meatus
- Posterior valves: use 5Fr anteriorly-curved catheter, can place finger in rectum to guide catheter if necessary
- Continent reservoir/pouch: overdistention may cause channel to kink, use cystoscope/ureteroscope to place guidewire, leave catheter for 1-2 weeks to heal
- Ileal conduit: can place catheter past stoma and inflate halfway, may need to secure to skin with stitch
- Artificial sphincter (AUS): avoid catheters if possible, place 12Fr if needed and remove as soon as possible to avoid erosion
- Difficult female catheters: place bed in trendelenberg and put pillow under hips to anteriorly elevate/tilt pelvis, have assistant retract labias laterally and anteriorly, can use coude to catch retracted urethral meatus, can place blindly over finger in vagina (will feel anterior vaginal wall between properly placed catheter and finger)
Post-obstructive diuresis (POD)
- Definition: UOP > 200mL/hr x2+ hrs or > 3L/d after removal of GU tract obstruction
- Physiologic diuresis: release of water/salt overload, resolves spontaneously
- Pathologic diuresis: continued high UOP due to loss of ADH feedback
- Hematuria: develops in 10% after relieving retention, may occasionally require clot irrigation
- No evidence/benefit to catheter clamping to prevent hematuria or POD
- Admit patient if AKI, electrolyte imbalance, or neurologic symptoms - monitor electrolytes
- If patient able to tolerate PO intake, regular salt/water balance with PO fluids
- If patient unable to tolerate PO intake, replete with 0.9% or 0.45% saline, repleting 50-80% UOP losses (avoids persistent fluid overload)
- Intermittent clamping: no proven benefit to intermittent clamping in RCT (Boettcher 2013), risk for hematuria is rare
References
- AUA Core Curriculum
- Boettcher, S., et al. "Urinary retention: benefit of gradual bladder decompression-myth or truth? A randomized controlled trial." Urologia internationalis 91.2 (2013): 140-144.
- Boone, T., J. Stewart, and L. Martinez. "Additional Therapies for Storage and Emptying Failure." Campbell-Walsh Urology 12 (2020).
- Daneshmand, Siamak, David Youssefzadeh, and Eila C. Skinner. "Review of techniques to remove a Foley catheter when the balloon does not deflate." Urology 59.1 (2002): 127-129.
- Jacob, J. and C. Sundaram. "Lower Urinary Tract Catheterization." Campbell-Walsh Urology 12 (2020).
- Villanueva, Carlos, and George P. Hemstreet III. "The approach to the difficult urethral catheterization among urology residents in the United States." International braz j urol 36 (2010): 710-717.
- Wieder JA: Pocket Guide to Urology. Sixth Edition. J.Wieder Medical: Oakland, CA, 2021.